Part II
2 History of Epidemiology
Learning Objectives
By the end of this chapter, the learner will be able to
-
Learn about the history of epidemiology, which parallels the history of public health
- Examine the history of epidemiology as a relatively new science
- Illustrate the history of epidemiology with events that not only happened in the traditionally European tradition, but also in the United States, and the Americas.
- Create a history of the field of epidemiology and public health in the United States.
Epidemiology: Classic historic events
The following content intends to provide only the most basic historical events in epidemiology. It does not intend to be exhaustive, but at least it will cover the most salient events that influenced the development of what it is known now as the field/science of epidemiology. From ancient civilizations, the time of the Greeks and Romans, and the 17th, 1800s, and 1990s to the 20th and 21st century the main purpose of epidemiology and public health has been the search for determinants that can explain causation and disease, the discovery of treatments and moreover, the prevention and control of disease, and related health problems
Although epidemiology is considered a new science, even before it was recognized as a science, it probably started in the times of the Greeks, who attributed disease causality to environmental factors influenced by the gods, the presence of epidemics, and the deadly toll of diseases were influenced by those factors. Also, at the time of the ancient Greeks, the disease was also explained by what is known as, the theory of the four ‘fluids’ (blood, phlegm, yellow bile, and black bile) that is, in turn, premised on the theory of the four elements (fire, earth, water, and air) and their four corresponding qualities (heat, dry, humid and cold).[1]
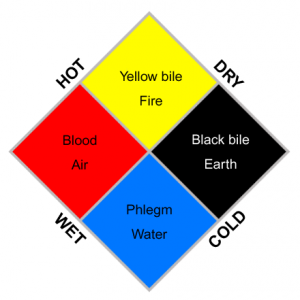 |
| Image of ‘the concepts of the four fluids/four elements’. Public Domain. Wikipedia. |
Early sanitation efforts, water systems and toilets
Then, the Romans, who developed aqueducts and sewage systems to prevent the development of diseases related to the lack of proper sanitation; brought water to their cities improved sanitation, and personal hygiene, which are essential for good health. [2]
 |
| ‘Pont du Gard’, By Benh LIEU SONG , CC BY-SA 3.0, Wikimedia. |
It is the Romans who also developed the first rudimentary system of disposition of excretas (or, excreta) before what we know as toilets were invented.[3]
 |
| ‘Ostia Toilets’(Ancient Roman latrines / latrinae), Public Domain,Wikimedia commons. |
Medieval period: The Black Death (or, Plague)
Then, the medieval period with the presence of deadly diseases such as the plague. [4]
 |
| ‘Citizens of Tournai bury plague victims,’ by Pierart dou Tielt, Wikimedia commons, Public Domain. |
Exercises
Before we continue with the history of public health. Check your Knowledge of what you just finished reading.
The Renaissance
With the advent of the sciences and arts during the Renaissance period, the initial work on medicine, and anatomic studies started. Several individuals flourished during those times, bringing new ideas, and discoveries including Girolamo Fracastoro (1478–1553), an Italian physician who introduced the term ‘fomites‘ still in use today in Epidemiology to refer to those inanimate objects that might contribute indirectly to the transmission of an infectious disease. And of course, the anatomical draws and notes done by Leonardo DaVinci were part of the contributions from this era. [5]
 |
| Image of ‘The Renaissance man’ by Leornardo DaVinci. Public Domain. |
If the history of medicine and epidemiology goes back to the beginning, there is a common factor for many events (that make history), they revolved around the search for causation, and how to prevent and treat disease. Since most deaths in earlier times of the humanity were caused mostly by infectious agents (usually bacteria), the progress in identifying these causes had to wait until the discovery of the microscope since most of these agents could not be seen with the naked eye.[6]
 |
| ‘Old-microscopes’. Image by Idal. Wikimedia Commons. Licensed CC BY-SA 3.0 Unported |
In this context, the first systematic methods used to identify causation are attributed to the father of medicine, Hippocrates who in about 400 years of the contemporary era was able to propose that there is a connection among three major elements of nature and health or disease, these are: air, water, and place (as we will see later in the book, place is usually referred as location – where people reside/live); he proposed for example that in some cases the ‘bad air’ can cause disease, or, the ‘quality of the waters’ as he called, and the place in which people live such as high altitudes and other geographical characteristics, especially the soil, and terrain.[7]
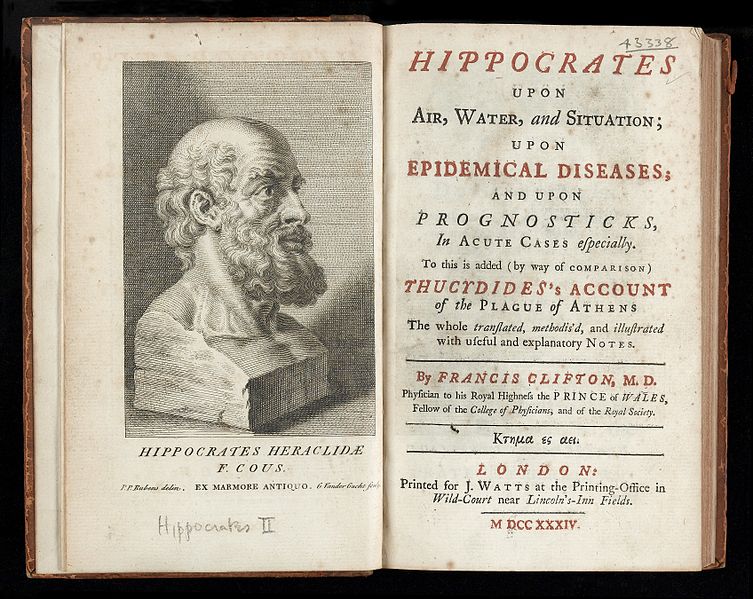 |
| ‘Hippocrates bust and title page’, image from Wikimedia Commons. Licensed CC BY 4.0 International. |
Another important person in the history of epidemiology is, John Graunt, a London cloth merchant who lived in the middle of the 17th century. Due to his work, he is considered the first demographer and initiator of the concept of vital statistics.John Graunt In 1603 in London, Graunt compiled the first register of births and deaths in England, under the name of, the ‘Bills of Mortality’. This is considered, the first systematic recording of deaths known in the history of record keeping and reporting of deaths, and other vital events. Graunt’s intentions were to show that human life conforms certain predictable statistical patterns, he wrote for example that deaths varied by age, sex, who died, of what, and where they died (the location), and when (the time of death). [8],[9]
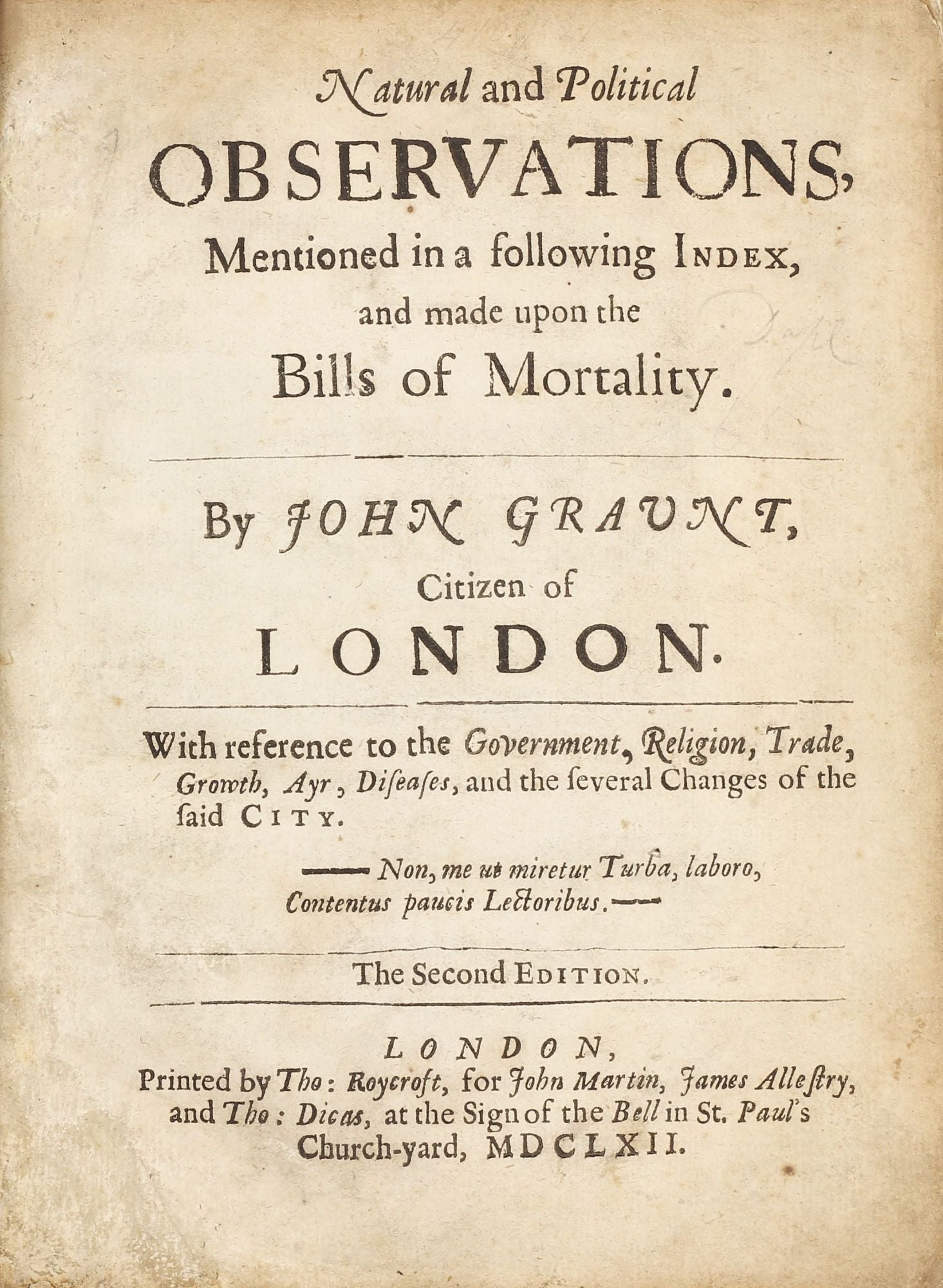 |
 |
| ‘The Bills of Mortality’, Image from Linda Hall Library. Public Domain. | John Graunt, Image from Wikimedia Commons. Public Domain. |
In the other in which events are presented here, the next person who made significant contributions to epidemiology and public health is Dr. John Snow – already discussed in another section of the chapter. One of the main remarks is that Dr. John Snow is considered the father of public health.
 |
| Dr. John Snow. Image from Wikimedia Commons. Public Domain. |
 |
| Dr. Snow’s map, image from Wikimedia Commons. Public Domain. |
Exercises
Before we continue with the history of public health. Check your Knowledge of what you just finished reading.Type your exercises here.
 |
| ‘The Duke of Orléans visiting the sick at the Hôtel-Dieu hospital, during the cholera outbreak, in 1832.’ Painting by Alfred Johannot, 1832. Licensed as Public Domain, from Musée Carnavalet. |
 |
| “The City of New Orleans and the Mississippi River c1885” Licensed Public Domain, Library of Congress. |
 |
| Dr. Robert Koch, image from Wikimedia Commons. Public Domain. |
Another individual who made a difference in the field of epidemiology is, William Farr, a British epidemiologist who was appointed compiler of abstracts in England, in 1839. His work examined the linkage between mortality rates and population density, it also created the foundation for the concept of vital statistics. Farr’s contributions provided the foundation for the classification of diseases (ICD system).[17]
 |
| ‘William Far’, image from Wikimedia Commons. Public Domain. |
 |
| Dr. Wade Hampton Frost, image from Wikimedia Commons. Public Domain. |
 |
| Dr. Alexander Langmuir, image from Wikimedia Commons. Public Domain. |
The history of epidemiology in the U.S. and England
The Parallel of the history of public health in England and the United States:
The history of public health in the United States also saw an event that marked the beginnings of what is essentially the beginning of public health in the U.S. This event is the publication of the Shattuck Report, written by Dr. Lemuel Shattuck and published in 1850 by the Massachusetts Sanitary Commission, it reports on the serious health problems experienced by certain groups of people, who were also living in unsanitary conditions in the city of Boston. Among the recommendations given to solve these problems, the report recommended the creation of a state health department and local boards of health in each town so public health interventions to address the issues were developed and implemented. [20],[21]
 |
| The Sanitary Commission of Massachusetts 1850, image from the Welcome Collection, Public Domain |
As a result (of the Shattuck’s report) in 1866 in New York City for the first time in the United States an organization as the report recommended was created. This is considered by many as the beginning of public health in the U.S. A picture of Dr. Shattuck is shown below:
 |
| Dr. Shattuck, image from London School of Hyg, & Trop. Med. |
Exercises
Before we continue with the history of public health. Check your Knowledge of what you just finished reading.
For example, Dr. John Snow (1884) in England, used epidemiological methods to identify the cause (origin) of the cholera epidemic that was killing thousands; and developed a strategy to stop the epidemic, which was basically removing the pump’s handle of the contaminated water source; in this manner, people would stop drinking the contaminated water, and the epidemic stopped.[23] See the image of the pump below:
 |
| “John Snow pump and pub” by mrlerone is licensed under CC BY-NC-ND 2.0 |
Seat belts law in the U.S.
A similar example can be found in the U.S. when the use of seat belts started as a public health measure to save lives during motor vehicle accidents, in the early 1970s when the measures were implemented, most people did not buckle up; they thought it was optional; but with the pass of time, people started seeing the benefits of seat belt use.[24] When the regulations are enforced, people who drive without a seat belt will get a traffic ticket from the police; and just because getting tickets is not pleasant, but also, just by knowing that the ticket is recompense for not wearing a seat belt, has made the measure very effective. It was probably the best way to make people use (consistently) seat belts while driving; and nowadays, it has become a habit, a norm. [25].
 |
“Seat Belts Have Saved an Estimated 255,000 Lives Since 1975,” Image from CDC. Public Domain.
Another parallel between England and the United States is the second wave of immigrants in the U.S.
Most books in epidemiology used the historical events of public health in England in order to draw a parallel with the U.S. history of public health; and this works well until we realize that the history of public health, and epidemiology in the U.S. has to do with one major issue, the wave of immigrants from distant countries, and how these immigrants dealt with the current sanitary conditions, housing, and environment conditions of their time, especially those immigrants who decided to reside in New York; which was not prepared to receive such high numbers of people, especially the unsanitary conditions of the buildings that many of these immigrants were allocated in the city. Crowdedness, lack of proper disposal of excreta, and high levels of cross-contamination of food, and water were typically in an Irish immigrant household (say, apartment) in New York. These immigrants faced a challenging time keeping themselves healthy and alive (especially their children, who in many cases died of dysentery, or any other type of oral-fecal-related disease. [26]
 |
| “New York, NY, yard of tenement (between 1900 and 1910)” Image from Library of Congress. Public Domain. |
Remarks
The early regulations started earlier in England, and the English people started hearing about the noxious effects of tobacco use (mainly smoking cigarettes) way before people in the U.S., and it was not until 1957 when this country (the U.S.) became aware of the need to study (do some research) the problem, and considered for the first time to start regulations on its use. In this regard, one of the main public health event on the noxious effects of tobacco is the released of the U.S. Surgeon General’s Advisory Committee on Smoking and Health report (on January 11, 1964), which concluded that cigarette smoking is a cause of lung cancer and laryngeal cancer in men, a probable cause of lung cancer in women, and the most important cause of chronic bronchitis.[29].
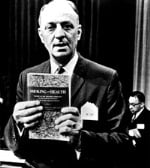 |
Picture of the 1964 U.S. Surgeon’s General Luther L. Terry, M.D., who released the first report on the nocebo effects of smoking on health. By CDC. Public domain.
|
In the search for the risk factors associated with Cardiovascular disease three major cohort studies have been conducted, these are, The Framingham Heart Study in Massachusetts, The Bogalusa Heart Study in Louisiana, and the San Antonio Heart Study in Texas. Each one of these studies will be briefly described in the following paragraphs, and more detailed information will be also provided in the chapter on study designs, and section on cohort studies.[30]
It represents one of the greater milestones in the epidemiology of cardiovascular disease studies in the U.S., and it also became well-known later in the world. The Framingham Heart Study (FHS) in Massachusetts, took its name from a town in eastern Massachusetts, U.S. which was selected as the site of the study. [31] See a picture of the Framingham City Hall below:
 |
“Town hall in Framingham, Mass.” Encyclopedia Britannica. EagleOne GNU Free Documentation License Version 1.2 |
The Framingham Heart Study is the first cohort to study the U.S. population on the issue of heart disease, and its related risk factors. It started in 1948 with a small group of individuals, and it is still collecting information about the white population in the U.S., and heart disease behavioral lifestyle risk factors. The findings of the Framingham Heart Study provided much of the common knowledge that people now have about heart disease, including the effects of exercise, diet, and smoking on cardiovascular disease.[32]
The Bogalusa Heart Study
Later in the history of epidemiology in the U.S., there was another major study focused on cardiovascular disease; but this time on the black population, its name the Bogalusa Heart Study, Bogalusa is a city (mainly black population) in Washington Parish, Louisiana, United States. It is the principal city of the Bogalusa Micropolitan Statistical Area, which includes all of Washington Parish and is also part of the larger New Orleans–Metairie–Hammond combined statistical area. [33]
See Louisiana Map below:
Bogalusa became well-known because of this study, which began in 1972 being the main investigator, Dr. Gerald S. Berenson, a Bogalusa native and pediatric cardiologist who recognized the need for investigations into the childhood antecedents of adult cardiovascular diseases.[34] I had the privilege to meet Dr. Berenson while doing my public health doctoral studies at Tulane University in New Orleans. [35]. To see additional images of the city of Bogalusa, see below:
 |
“Bogalusa City Hall“. Wikimedia Commons. Licensed CC BY-SA 4.0 |
The main contributions of the Bogalusa Heart Study among others include the following: adult heart disease, atherosclerosis, coronary heart disease, and essential hypertension begin in childhood. Cardiovascular risk factors can be identified in early life, but the levels of risk factors in childhood are different than those in the adult years. In addition, another great contribution of the Bogalusa Heart Study among others is that it is targeted (collected data) to African American children (while the Framingham targeted mainly adults). [36]
The next step, the San Antonio Heart Study (SAHS)
With the past of time, the need to have information (data) about cardiovascular disease among another major ethnic group in the U.S. became one of the major reasons to conduct another famous cohort study on the Latino/Hispanic population in the U.S. The name of the study, is San Antonio Heart Study, San Antonio, Texas. See a picture of San Antonio below:
 |
“Downtown San Antonio.” Wikimedia Commons. CC BY-SA 3.0 |
My personal critique/comments of the San Antonio Heart study is that it lacks representativity of the different U.S. Latino ethnic groups, by being mainly focused on Mexican-American, which constitute a great majority of the population of Latinos in the U.S. and excluding the great numbers of new Latino immigrants from other countries, and regions especially Central America and the Caribbean, the data results cannot be generalized to the rest of the U.S. Latino population in the U.S., but on the positive side, the contribution of the San Antonio Heart Study (SAHS) cannot be denied because it represents pioneering research on two major problems (cardiovascular disease and type II diabetes) of morbidity, and mortality among the U.S. Latino population.
Key Takeaways
Medical and Public Health Research going wrong in the U.S., the case of the Tuskegee syphilis study
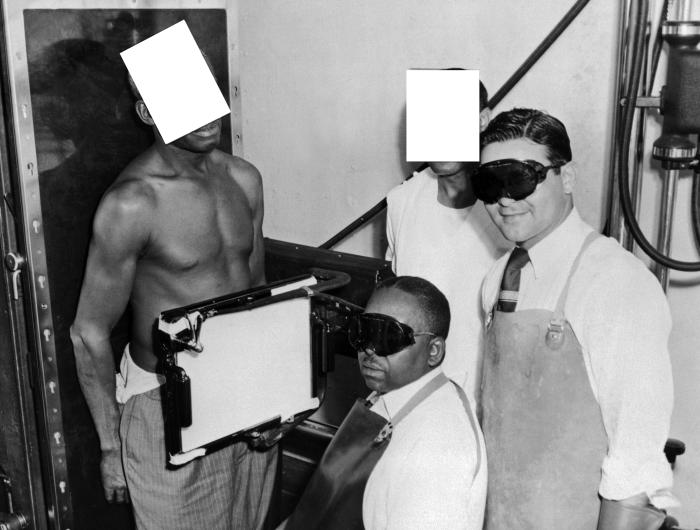 |
| Image from CDC Public Health Image Library (PHIL). |
According to the CDC, this photograph was taken around 1932, it shows participants in the Tuskegee Syphilis Study. In this picture, an African-American man was being X-rayed, while in the standing position.
At the beginning of the study, the number of participants included 600 African-American men, from this group, 399 had syphilis and 201 did not have the disease. During the time of the study, the investigators told these men that were being treated by “bad blood,” a common term at that time that was used to describe some common diseases such as syphilis, anemia, and fatigue. The study lasted for 40 years, although the men participating in the study, were told that the study would last 6 months.[39]
The Tuskegee syphilis study is an example of human experimentation on the clinical history of a common infectious disease which by that time had treatment already available. The withholding of the treatment exposed the study participants, their families, and generations of African Americans in the South to syphilis. For this reason, this study is frequently cited as an example of what an investigator is not supposed to do in conducting research, especially research on human subjects. The question that usually comes to mind when the author reads about this study is, what can be done to prevent similar situations in the future of research in the U.S.? And the question remains open.
The epidemic of smallpox in Europe and then, later in the United States
From the list of plagues that affected the world population in the past, one of the major problems is smallpox, a disease now eradicated. A disease caused by the Variola virus . It caused millions of deaths especially during the Medieval times, although it is believed to have existed for at least 3000 years. [40]
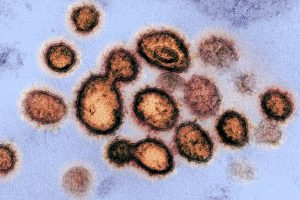
 |
| “Variola virus” image from CDC/ Dr. Fred Murphy; Sylvia Whitfield, Public domain, via Wikimedia Commons |
The person who created the first smallpox vaccine was Dr. Edward Jenner, an English doctor who as part of his observations noted that milkmaids who had gotten cowpox were protected from smallpox, which means that they received immunity (this concept was unknown at his time) from having the disease, this became the base for the development of the smallpox vaccine. Having a vaccine made a tremendous difference in the history of the disease, which basically contributed to its eradication. [41], [42]
 |
| “Edward Jenner (1749–1823), Public Domain, from the National Library of Medicine |
Smallpox was mainly a European problem for a long time, until the colonization of the new world (America) in which the colonizers brought the disease to the natives, which did not have immunity since they were never exposed to the smallpox agent. So, smallpox killed thousands of natives (not only in what is known as North America today but also in the Caribbean and South America. One of the worst examples is the killing of Native Americans in the United States when the colonizer gave (as a gift, at least once) blankets intentionally contaminated with smallpox – this is also an example of an early episode of terrorism using biological weapons, as it was expected the strategy worked, and again entire populations of Native Americans were killed by the disease. [43]
 |
| “Treaty of Penn with Indians by Benjamin West”, Public Domain Wikimedia Commons. |
The history of epidemiology and public health has been shaped by the presence of pandemics: plague, flu, and recently, coronavirus or, COVID-19. Throughout history, these pandemics have been responsible for the death of thousands of people around the world. Overall, what has changed from ancient times to today’s public health is the availability of vaccines, and the improvement in water and sanitation around the world, with major gains for developed nations who have better systems of drinking water, and sanitation. Until recently, the fear of a major pandemic has been for a worldwide-scale flu that could kill thousands of people. But instead of the flu, the world received the coronavirus pandemic, which is still around. Since flu has been the major fear before the coronavirus, this section will cover some of the major events of flu pandemics.
Flu pandemics
In general, flu pandemics have been repeated in history every 100 years, and because of that the ‘expected’ and ‘predicted’ pandemic was on flu (and not coronavirus).[44]. Because of its importance in history, the first major pandemic that appears usually in most history books is the flu pandemic.
The flu pandemic of 1918
The 1918 Influenza (flu) Pandemic (also called, the Spanish flu, because of the great mortality in that country at that time). This famous pandemic lasted from 1918-1919 and killed 50 to 100 million persons worldwide. The pandemic had three waves as it is represented in the following image:
 |
|
“1918 spanish flu waves,” Image Licensed Public Domain, Wikipedia. |
The 2009 H1N1 influenza pandemic: a repeat of the 1919 pandemic
The specific time of this pandemic is from 2009-2010. The disease was first identified in the United States and eventually was named the 2009 H1N1 influenza. The first two cases of the disease were reported by the Centers for Disease Control and Prevention (CDC) in April 2009, after this, the number of cases grew to 60 million by summer 2010. The pandemic also attacked several other countries in the world, and it was known to prefer the group of people 14-64 years, with those aged 65 and older as the less affected group.[47], [48] This pandemic should have served as a lesson for the U.S., but a lot of skepticism grew that the possible for another major pandemic was not possible, or, if this would happen then, the country had enough public health resources including vaccines to control the problem, which has been proven wrong with the current coronavirus pandemic making manifest that the U.S. public health system was not prepared for a pandemic.
 |
The prediction of a new pandemic was always there but the medical and public health preparations were never in place, so, the pandemic started in Wuhan, China with several infected persons never seen before, the agent coronavirus named COVID-19 because of the year in which it was reported as the cause of the pandemic. The news was everywhere, but the United States did not pay attention to the situation, until almost two months later in March 2020; acknowledging and responding to the pandemic was proven bad, because the country and the world did not have a vaccine for it, nor the U.S. had the public health infrastructure to respond properly, there was a lot of unknown about the disease, and especially its form of transmission; the measures taken since the beginning did not have a social acceptance in a society that values so much its personal freedom, and having the federal government, and public health authorities, and experts tell the public to wear a mask, stay at home and related mandates created an epidemic of misinformation, and contradictory messages that have been hard to eliminate until today.[51],[52]. I have found an image -shown below that summarizes some of the reasons for this campaign of misinformation that has been one of the major problems of the COVID-19 pandemic.
 |
| “Fast-Slow-Science,” By Dasaptaerwin, Licensed CC 4.0 International, Wikimedia Commons. There is also an article that refers to more details about the content of the image.[53] |
 |
| “Novel Coronavirus SARS-CoV-2 (or, COVID-19) electronic microscope image,” The National Institute of Allergy and Infectious Diseases, Licensed Public Domain. |
 |
| “Global distribution of estimated excess mortality rate due to the COVID-19 pandemic, for the cumulative period 2020–21” Image from an article by Haidong Wang, H., Paulson, KR., Pease, SA., Watson, S. et al.[57] |
Summary
Although a historical review of events, and individuals, it shows that the history of public health and epidemiology are intertwined. The historical events mentioned in this chapter confirm that epidemiology as a science has made great contributions to medicine and public health, in the search for determinants and the design of effective public health interventions.
- Yannis T. (2009). The historical origins of the basic concepts of health promotion and education: the role of ancient Greek philosophy and medicine, Health Promotion International, 24 (2), 185–192. From https://doi.org/10.1093/heapro/dap006 ↵
- Deming D. (2020). The Aqueducts and Water Supply of Ancient Rome. Ground water, 58(1), 152–161. https://doi.org/10.1111/gwat.12958 ↵
- Gill, N.S. (August 02, 2019). Roman Baths and Hygiene in Ancient Rome. ThoughtCo. From https://www.thoughtco.com/hygiene-in-ancient-rome-and-baths-119136 ↵
- ‘Black Death,’ Wikipedia, licensed Creative Commons Attribution-ShareAlike License 3.0 URL: https://en.wikipedia.org/wiki/Black_Death ↵
- MNT Editorial Team. (Feb. 8, 2022). What was medieval and Renaissance medicine? Medical News Today (MNT). From https://www.medicalnewstoday.com/articles/323533 ↵
- Poppick, L. (March 30, 2017). Let Us Now Praise the Invention of the Microscope In Smithsonian Magazine. Available at: https://www.smithsonianmag.com/science-nature/what-we-owe-to-the-invention-microscope-180962725/ ↵
- Centers for Disease Control and Prevention (CDC). (n.d.). Lesson 1: Introduction to Epidemiology Section 2: Historical Evolution of Epidemiology. Circa 400 B.C. section. Available at https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section2.html ↵
- Stephan, E. (n.d.). John Graunt (1620-1674), Observations in the Bills of Mortality. From http://www.edstephan.org/Graunt/graunt.html ↵
- Linda Hall Library. (2020, April 24). Scientist of the Day - John Graunt. From https://www.lindahall.org/john-graunt/ ↵
- Kneisl, K. (February 9, 2021). John Snow, A Turning Point In Epidemiology. From https://storymaps.arcgis.com/stories/1913fb6e17cd49c88b801e4c6edb67bf ↵
- University of California Los Angeles (UCLA). (2003). Who is John Snow? UCLA Dept. of Epidemiology, Fielding School of Public Health. From http://www.ph.ucla.edu/epi/snow.html ↵
- No author. (April 23, 2020). "Careless of Cholera": The New Orleans Outbreak of 1848. The Times Picayune. From https://www.pitothouse.org/blog/2020/4/23/careless-of-cholera-the-new-orleans-outbreak-of- 1848 ↵
- No author. (2020). History of Tulane SPHTM, a Timeline. From https://sph.tulane.edu/timeline ↵
- Segre J. A. (2013). What does it take to satisfy Koch's postulates two centuries later? Microbial genomics and Propionibacteria acnes. The Journal of investigative dermatology, 133(9), 2141–2142. From https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3775492/ ↵
- Snow, J. (1855). On the Mode of Communication of Cholera. From http://www.ph.ucla.edu/epi/snow/snowbook_a2.html ↵
- Rogers HR.(1895). Dr. Robert Koch and His Germ Theory of Cholera. JAMA, XXIV(23):903–904. doi:10.1001/jama.1895.02430230037013 ↵
- Lilienfeld, DE. (2007). Celebration: William Farr (1807–1883)—an appreciation on the 200th anniversary of his birth. International Journal of Epidemiology, 36(5), 985–987. From https://academic.oup.com/ije/article/36/5/985/775018 ↵
- Johns Hopkins Bloomberg School of Public Health. (December 20, 2012). Medical Historian Speaks at School about Wade Hampton Frost (web article). From https://publichealth.jhu.edu/2004/frost ↵
- Thacker, SB. (n.d.). Epidemiology and Public Health at CDC. Office of Workplace and Career Development, Office of the Director. From https://www.cdc.gov/mmwr/preview/mmwrhtml/su5502a2.htm ↵
- Report of the Sanitary Commission of Massachusetts 1850. Report available in pdf from https://www.google.com/search?client=firefox-b-1-d&q=the+shattuck+report ↵
- Winkelstein, W. (July 2008). Lemuel Shattuck Architect of American Public Health. Epidemiology, 19(4), 634. From https://journals.lww.com/epidem/Fulltext/2008/07000/Lemuel_Shattuck__Architect_of_American_Public.21.aspx ↵
- Britannica. (n.d.). National developments in the 18th and 19th centuries. From https://www.britannica.com/topic/public-health/National-developments-in-the-18th-and-19th-centuries ↵
- University of California Los Angeles (UCLA). (2003). John Snow and the Broad Street Pump. UCLA Dept. of Epidemiology. From https://www.ph.ucla.edu/epi/snow/snowcricketarticle.html ↵
- Centers for Disease Control and Prevention. (n.d.). Policy Impact: Seat Belts. From https://www.cdc.gov/transportationsafety/seatbeltbrief/index.html ↵
- Dept of Transportation (US), National Highway Traffic Safety Administration (NHTSA). (2010). Traffic Safety Facts: Seat Belt Use in 2010—Overall Results. Washington (DC): NHTSA. From http://www-nrd.nhtsa.dot.gov/Pubs/811378.pdfpdf icon ↵
- Library of Congress. (n.d.). Adaptation and Assimilation. Presentation, Immigration and Relocation in U.S. History. From https://www.loc.gov/classroom-materials/immigration/irish/adaptation-and-assimilation/ ↵
- Markel, H., & Stern, A. M. (2002). The foreignness of germs: the persistent association of immigrants and disease in American society. The Milbank quarterly, 80(4), 757–v. https://doi.org/10.1111/1468-0009.00030 From https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7152289/ ↵
- Comments of the author. ↵
- Centers for Disease Control and Prevention. (n.d.). History of the Surgeon General’s Reports on Smoking and Health. From https://www.cdc.gov/tobacco/data_statistics/sgr/history/index.htm ↵
- See the cohort studies section in chapter 5. ↵
- Bacallao Gallestey, J. (n.d). Framingham Heart Study research project, Framingham, Massachusetts, United States. Encyclopedia Britannica. From https://www.britannica.com/event/Framingham-Heart-Studay ↵
- No Author. (n.d.). Framingham Heart Study, Participant cohorts. Available at https://www.framinghamheartstudy.org/participants/participant-cohorts/ ↵
- Bogalusa Louisiana. From Wikipedia, https://en.wikipedia.org/wiki/Bogalusa,_Louisiana ↵
- No Author. (n.d.). Bogalusa Heart Study. Available at: https://www.clersite.org/bogalusaheartstudy/ ↵
- Personal comments from the author. ↵
- Tulane Center for Lifespam Epidemiology Research (CLER). (n.d.). Bogalusa Heart Study. Available at: https://www.clersite.org/bogalusaheartstudy/ ↵
- Shen D, Mitchell B, Hazuda H, Clark G, and Stern M. (1992). The San Antonio heart study research information study, Proceedings Computers in Cardiology, 607-610. Available at: https://ieeexplore.ieee.org/document/269385/keywords#keywords ↵
- CDC. (n.d.). The U.S. Public Health Service Syphilis Study at Tuskegee. From https://www.cdc.gov/tuskegee/index.html ↵
- National Archives of Atlanta. (n.d.). Tuskegee Syphilis Study. From https://www.archives.gov/atlanta/exhibits/item470-exh.html ↵
- World Health Organization (WHO). (No date). Smallpox. From https://www.who.int/health-topics/smallpox#tab=tab_1 ↵
- Riedel S. (2005). Edward Jenner and the history of smallpox and vaccination. Proceedings (Baylor University. Medical Center), 18(1), 21–25. https://doi.org/10.1080/08998280.2005.11928028 ↵
- CDC. (No date). History of Smallpox. From https://www.cdc.gov/smallpox/history/history.html ↵
- Kiger, PJ. (Nov 25, 2019). Did Colonists Give Infected Blankets to Native Americans as Biological Warfare? There’s evidence that British colonists in 18th-century America gave Native Americans smallpox-infected blankets at least once—but did it work? History, 15. From https://www.history.com/news/colonists-native-americans-smallpox-blankets ↵
- Kertscher, T. (April 10, 2020). Fact-check: Has a pandemic occurred every 100 years? PolitiFact. From https://www.statesman.com/story/news/politics/elections/2020/04/10/fact-check-has-pandemic-occurred-every-100-years/984128007/ ↵
- Taubenberger, J. K., & Morens, D. M. (2006). 1918 Influenza: the mother of all pandemics. Emerging infectious diseases, 12(1), 15–22. https://doi.org/10.3201/eid1201.050979 ↵
- Barry, J. M. (2020). The great influenza: The story of the deadliest pandemic in history. Penguin UK. ↵
- CDC. (no date). 2009 H1N1 Pandemic (H1N1pdm09 virus). From https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html ↵
- Mayo Clinic Staff. (Feb 24, 2021). H1N1 flu (swine flu). From https://www.mayoclinic.org/diseases-conditions/swine-flu/symptoms-causes/syc-20378103 ↵
- Branswell, H. (June 11, 2019). The last pandemic was a ‘quiet killer.’ Ten years after swine flu, no one can predict the next one. STAT, Health. From https://www.statnews.com/2019/06/11/h1n1-swine-flu-10-years-later/ ↵
- Osterholm, MT., Kelley, NS., Manske, JM., Ballering, KS., Leighton, TR. (October 2012). CIDRAP Comprehensive Influenza Vaccine Initiative report. University of Minnesota, Academic Health Center. From https://www.cidrap.umn.edu/sites/default/files/public/downloads/ccivi_report.pdf ↵
- Tagliabue,F.,Galassi,L., Mariani,P.(2020). The “Pandemic” of Disinformation in COVID-19. SN Comprehensive Clinical Medicine, 2 (9),1287. From https://doi.org/10.1007/s42399-020-00439-1 ↵
- Grimes, DR. (March 12, 2021). Medical disinformation and the unviable nature of COVID-19 conspiracy theories. PLOS One (Pone). From https://doi.org/10.1371/journal.pone.0245900 ↵
- Dunleavy, Daniel, & Hendricks, Vincent. (2020, September 28). Fast Science, Slow Science: Finding Balance in the Time of COVID-19 and the Age of Misinformation (Version 1). Zenodo. http://doi.org/10.5281/zenodo.4056909 ↵
- Smriti Mallapaty, S. (28 January 2022). Where did Omicron come from? Three key theories The highly transmissible variant emerged with a host of unusual mutations. Now scientists are trying to work out how it evolved. Nature. From https://www.nature.com/articles/d41586-022-00215-2 ↵
- Haidong Wang, H., Paulson, KR., Pease, SA., Watson, S. et al. (April 16, 2022). Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet, 399 (10334), 1513. From https://doi.org/10.1016/S0140-6736(21)02796-3 ↵
- No author. (No date). Johns Hopkins University Coronavirus Resource Center. From https://coronavirus.jhu.edu/map.html ↵
- aidong Wang, H., Paulson, KR., Pease, SA., Watson, S. et al. (April 16, 2022). Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet, 399 (10334), 1513. From https://doi.org/10.1016/S0140-6736(21)02796-3 ↵
Term commonly used for the disposal of urine and feces.
it refers to inanimate objects that may be contaminated with the infectious agent
the term that refers main to disease etiology (cause)
Considered the father of medicine as a science.
considered the first demographer
He is considered the father of public health.
A map that is developed using GIS software in which data are represented by dots (the pixels in the image).
geographic information system, which is a series of software and computers used to model data that is represented by dot maps - see definition of a dot map in this section of the book.
A choropleth map is a type of thematic map in which a set of pre-defined areas is colored or patterned in proportion to a statistical variable.
International Classification of Diseases, it uses specific coding systems to classify diseases, so, international comparisons can be established.
The act of planning a system for something, or of organizing something in a system - Cambridge Dictionary online: https://dictionary.cambridge.org/
A figure of speech that means, 'similar' or, 'analogous' to another. A comparison.
The term eradicated is used to refer to infectious diseases that do not longer exist due to public health efforts mainly vaccinations.

Feedback/Errata