Other Health Disabilities
The special education category of “Other Health Disabilities” (OHD) in Minnesota has shown consistent annual growth since data collection began in 1990–91. This growth can be attributed to various factors such as advancements in healthcare that have improved survival rates and increased life expectancy for infants and students with chronic or acute health conditions. As a result, a larger population of students requires specialized educational and healthcare services. Additionally, the current understanding and recognition of disabilities have improved, leading to better identification and classification of students under the OHD category. Increased awareness and accessible special education services have likely contributed to such growth, ensuring that students with OHD receive the necessary support and accommodations. Figure 1 helps us visualize the growth of OHD.
Figure 1
Other Health Disabilities – MN Unduplicated Child Count
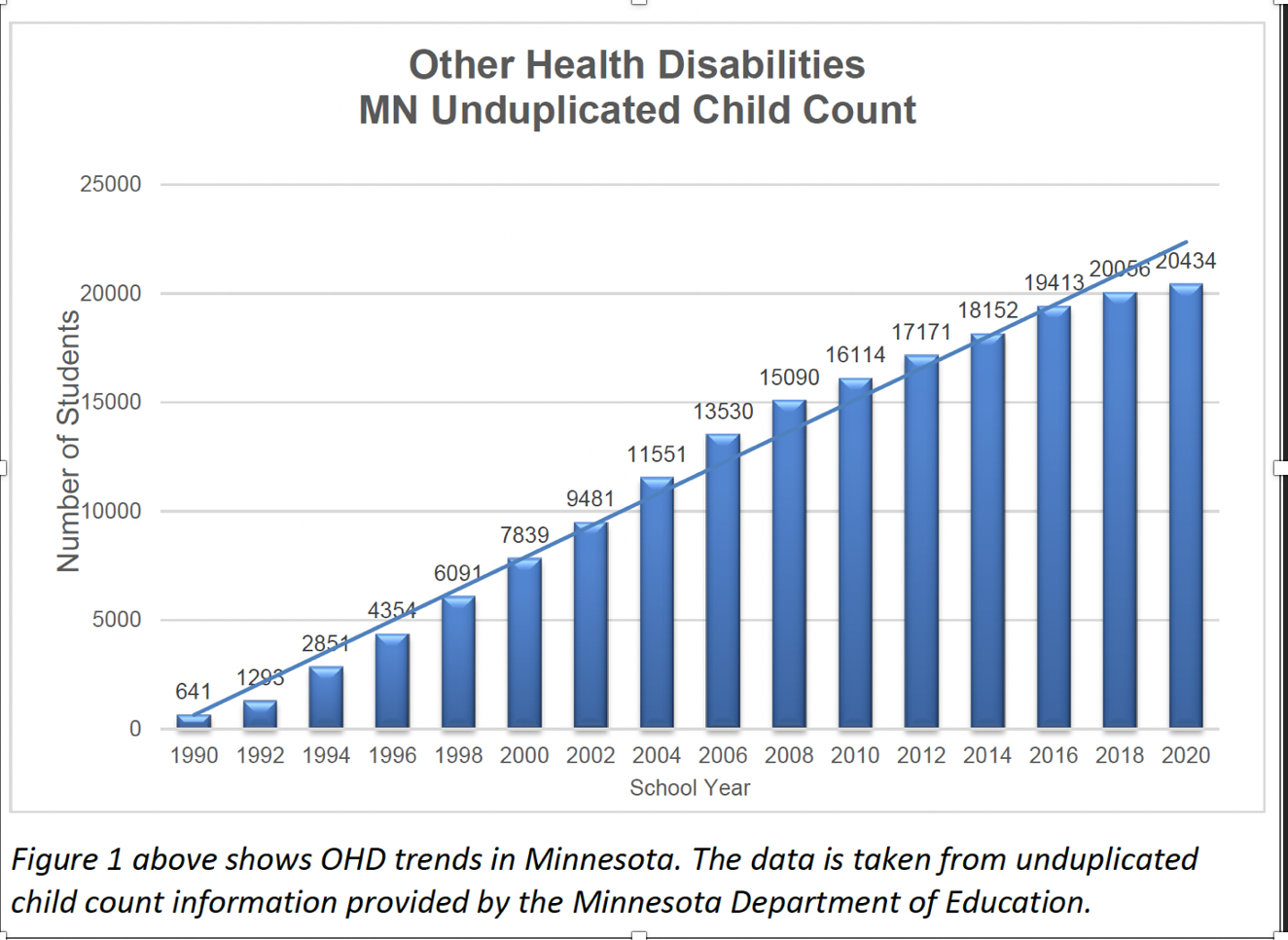
Note. The data in this figure are taken from unduplicated child count information provided by the Minnesota Department of Education.
In recent years, the definition and interpretation of OHD have evolved, leading to a significant increase in the OHD child count in Minnesota. Including Attention Deficit/Hyperactivity Disorder (ADHD) under the OHD category in 2001 has played a significant role in this increase. ADHD will not be covered in this chapter; instead, see Chapter 6. Moreover, there has been a perceptual shift in the educational and medical communities regarding what constitutes a chronic or acute health condition. This shift has raised questions about whether specific medically diagnosed mental health and neurobiological conditions should be considered for special education eligibility under OHD. A diverse range of conditions can lead to OHD. Medical conditions associated with OHD include:
Educators must grapple with how to serve best these unique students, who often present complex symptoms and require specific educational interventions to address their needs effectively. It is crucial to adapt policies, guidelines, and support systems to meet the evolving requirements of students with OHD to ensure their educational success.
Identification
When a student has a documented medical diagnosis of a chronic or acute health condition that raises educational concerns, a comprehensive evaluation should be conducted that does not solely focus on their health condition but also considers their identified educational needs that are impacted by the condition. Even students with the same health condition can exhibit different symptoms, needs, and strengths. The evaluation team must recognize and address these individual differences. Medical professional documentation is not only helpful but required. According to Minnesota Rule 3525.1335, when an OHD disability is suspected, there needs to be written and signed documentation from a medical professional who addresses the following topics: (1) outlining activity limitations or restrictions, (2) discussing implications for school attendance (such as anticipated absences due to hospitalizations or surgeries), (3) specifying medications or specialized healthcare procedures required during the school day, and (4) identifying medications that may have adverse effects on school performance.
The following examples of students with OHD demonstrate the variability within this disability category and the unique needs of students, as compared to their non-disabled peers:
- Jamal’s leukemia causes frequent absences from school. He has missed 36% of the last 80 days in the hospital or at home due to chemotherapy and the need to be isolated from infection. During those absences, Jamal has missed significant instruction time in all subject areas. Classmates have missed an average of 4% of the last 80 days.
- Alicia’s health condition requires two specialized treatments each day while at school. Her trips to and from the health office and the treatments take 15–20 minutes each time. The teacher reports that Alicia has difficulty completing classroom assignments in class. When Alicia takes assignments home, she misses the teacher’s help. Her classmates can finish classroom assignments in class.
- Owen’s health condition requires specific medications that can affect his short-term memory as well as auditory and visual processing speed. As a result, he has difficulty learning and retaining new information taught in algebra, following verbal directions in a time-efficient manner, and absorbing meaning from written texts. During an observation, he took 15 minutes to read and answer three math questions. The three control students took three, six, and seven minutes for the same questions.
- Moua’s health condition causes limited strength and difficulty handling books and writing implements. His peers hold and use these materials easily. This difficulty has resulted in Moua falling behind his peers regarding task initiation and completion.
- Abdi’s health condition results in limited endurance and stamina. He often needs to stop his work and rest in class or go to the health office for a nap. As a result, he has completed two out of 15 writing assignments. His classmates have completed an average of 13 out of 15.
- Leticia’s seizure disorder makes it difficult for her to maintain focus. During an observation in history class, she had three or more absence seizures in one hour. Her attention can suddenly change for a few seconds, and she stares ahead. The three occasions that the observer noted were when Leticia did not respond to the teacher calling her name, to her pencil dropping on the floor, and to the bell signaling the end of class. In comparison, her classmates responded when the teacher called on them and when the bell rang. Two students turned when Leticia dropped her pencil. The seizures interfere with her ability to hear verbal directions and instructional content, directly impacting her academic performance.
- Noah’s health interferes with his ability to organize and manage his materials. Over the last two months (40 days), he misplaced 39 out of 46 homework assignments, could not find his pencil for 36 out of 40 days, and forgot his library book for two out of eight days. In contrast, two control classmates misplaced four and six out of 46 homework assignments, could not find their pencils two and nine out of 40 days, and forgot their library books two and no days, respectively.
- Sergei’s health condition interferes with completing activity-based classroom projects within the required time. Two out of the six science projects were on time. Eighty percent of his classmates turned their classroom projects in by the due date.
The evaluation process can be complex when determining eligibility for students with mental health conditions and dual diagnoses. Unlike heart conditions, epilepsy, or diabetes, mental health conditions often involve multiple variables that must be carefully considered. Additionally, team members may have different opinions regarding the most appropriate special education category to address the student’s educational needs, particularly when aligning mental health diagnoses with the Emotional/Behavioral Disorders (E/BD) category. The team’s primary focus should be on identifying the student’s educational needs and determining the category that best addresses those needs.
It is also important to note that some students with health conditions may utilize accommodations, are academically successful in the school setting, and do not require special education services. These students may be most appropriately served under a Section 504 Plan, which documents the accommodations necessary for successful participation in the general education setting.
OHD vs. PI
The eligibility criteria for students with PI and OHD both require a medical diagnosis. Still, they differ regarding the specific conditions and their impact on physical and academic functioning. A physical impairment is a diagnosed chronic physical impairment that affects functioning, whereas a health disability involves a chronic or acute health condition that impacts school functioning. Students with physical impairments may also have secondary health issues related to their condition. If the health disability is related to the physical impairment and the student meets PI criteria, PI should be considered the primary category. However, complex situations with both conditions require a decision by the educational team. In Minnesota, secondary categories are no longer officially recognized, but some districts use them for educational planning. A P/HD teacher is also required for students with physical impairments, but OHD has no mandatory teacher licensure. However, involving a P/HD teacher for students with OHD and chronic health conditions can enhance support and expertise.
Characteristics
Students with chronic health conditions may face numerous challenges that impact their academic performance and overall school experience. These challenges include underachievement compared to their peers without health conditions (despite often typical intelligence) primarily due to sporadic or chronic absenteeism, frequent medical appointments or hospitalizations, and missed instructional time. Medication side effects can also affect a student’s ability to stay alert and focused, leading to comprehension, memory, and attention difficulties.
In addition, physical effects such as pain, nausea, and fatigue can further hinder a student’s learning and concentration. Medications and treatments may have an adverse impact on memory and comprehension abilities as well. Moreover, physical changes resulting from health conditions, such as hair loss or burn scars, can lead to concerns about peer reactions and can potentially affect a student’s self-esteem and social interactions. The combination of missed school, social activities, physical discomfort, potential teasing, and uncertainty about the future can significantly impact the social-emotional well-being of these students.
Recognizing the multifaceted impact of a student’s medical condition and related symptoms on their educational performance, including academic, social, adaptive, and functional aspects, is crucial. By understanding these challenges, educators, healthcare professionals, and support systems can provide appropriate interventions and accommodations to help students with chronic health conditions thrive academically and emotionally.
Supporting Student Success
In Minnesota, there is no specific teacher licensure for OHD. However, it is recommended that an educator with knowledge and expertise in OHD be included in developing the evaluation plan when a student has a documented medical diagnosis of a chronic or acute health condition that raises educational concerns. This educator, such as an OHD consultant or specialist, is vital in helping the evaluation team determine whether the student is eligible for special education services. They also actively participate in creating an Individual Education Plan (IEP) and serve as an ongoing member of the IEP team.
Although there is no specific licensure for OHD, there are situations in which it may be appropriate for a PI teacher to be involved with a student who meets OHD criteria due to a chronic health condition that impacts their learning. PI teachers possess expertise and training that can enhance support provided to the student and school team. Examples of such chronic health conditions include cancer, rheumatoid arthritis, cystic fibrosis, and others. By incorporating the specialized knowledge of P/HD teachers, the school team can better address the educational needs of students with OHD and ensure that their individualized support is comprehensive and effective.
IEP Goals
IEP goals and objectives play a crucial role in addressing the educational needs of students, especially those with chronic medical conditions. These needs encompass various domains beyond academics and are essential in fostering independence within the educational setting. For instance, goals may focus on developing organization and planning abilities, promoting the independent completion of tasks, enhancing study skills, fostering self-management skills, and empowering students to advocate for themselves about their disabilities. Additionally, goals can include acquiring compensatory skills, such as effectively utilizing assistive technology, which can support students’ overall educational progress and success. By incorporating these diverse areas of need into the IEP, educators can provide comprehensive support and empower students to thrive in their educational journeys.
Service Delivery Models
When a student qualifies for special education services under the OHD category, the IEP team is responsible for determining the provision of direct and indirect services based on the student’s instructional needs related to their chronic or acute health condition. Direct services involve OHD specialists, special education teachers, or related service professionals (e.g., speech-language pathologists, occupational therapists, or physical therapists) who deliver instruction that other educational team members cannot replicate. A collaborative instructional model must be prioritized whenever feasible and must involve other classroom staff in the instructional process. This partnership is crucial for various aspects such as core academic content instruction, organizational strategies, work completion, and fostering the development of self-advocacy skills in the student. By working together, the team can ensure comprehensive and effective support for the student’s educational journey.
Indirect services refer to various support activities and accommodations provided to a student with special needs. These services are not directly delivered to the student but are designed to facilitate their educational progress and enhance their learning experience. Examples of indirect services for students with OHD include:
- Ongoing progress reviews: Conducting regular assessments and evaluations to monitor the student’s academic and developmental progress
- Cooperative planning: Collaboration among educators, specialists, and parents to develop strategies, set goals, and design instructional plans tailored to the student’s individual needs
- Consultation: Expert advice and guidance provided by professionals to teachers and support staff regarding effective instructional methods, behavior management techniques, or specific accommodations for the student
- Demonstration teaching: Providing instructional demonstrations and modeling techniques to educators, helping them understand and implement effective teaching strategies for the student
- Modification and adaptation of the environment, curriculum, materials, or equipment: adjusting the learning environment, curriculum content, teaching materials, or specialized equipment to ensure the student’s access and participation in educational activities
- Direct contact with the pupil to monitor and observe: Occasional or periodic observations and interactions with the student to assess their progress, evaluate the effectiveness of the provided accommodations, and identify areas for further support or adjustment
Adaptations
Adaptations and accommodations are crucial components of an IEP for students with OHD. These accommodations are designed to meet the unique needs of students with chronic or acute health disabilities and ensure their educational success. Special educators with knowledge of the student’s areas of need are vital in providing guidance and support when determining appropriate accommodations.
Accommodations include supplementary aids and services, classroom and testing accommodations, support for school personnel, and individual accommodations for state or district testing. They aim to provide necessary assistance and adjustments to enable students with OHD to participate fully in the educational environment. Examples of accommodations for students with OHD may include:
- Individualized health plans (IHP): A comprehensive plan outlining the student’s health needs, emergency protocols, medication administration, and other relevant health-related information
- Emergency evacuation plans: A customized plan detailing the procedures to safely evacuate students during emergencies, considering their specific health conditions and mobility limitations
- Modified school schedules: Adjusting the student’s daily timetable to accommodate medical treatments, therapies, or appointments
- Accommodations to address auditory or visual distractions: Providing strategies such as preferential seating, noise-canceling headphones, or visual aids to minimize distractions and enhance focus
- Testing accommodations: Modifying assessment conditions, such as extended time, breaks, or providing a quiet testing environment, to ensure students’ equal participation and access to demonstrate their knowledge
- Extended assignment due dates: Allowing additional time for completing assignments, considering the impact of medical absences or related challenges
- Alternate response or assignment formats: Allowing students to express their understanding or knowledge through alternative means such as oral presentations, visual projects, or assistive technology
- Additional adult support: Providing a paraprofessional or aide to assist students with OHD in the classroom, ensuring that they receive personalized attention and guidance
- Access to adaptive equipment and assistive technology: Providing specialized tools, devices, or software that assist students with OHD in learning and communication
- Alternate instructional settings (home, hospital): Arranging for education to be delivered in alternative settings when a student’s health condition prevents regular attendance at school such as homebound or hospital-based instruction.
These examples illustrate the wide range of accommodations that can be implemented to support students with OHD, promoting their academic progress and addressing their individual needs in the educational setting.
To learn more about supporting students with OHD, their families, and educators, check out: Other Health Disabilities Resources
Note: The information shared in this section was remixed from Special Education Evaluation and Services for Students with Other Health Disabilities: A Manual for Minnesota Educators; Updated 2018.
Think, Write, Share
- Create two to three tip sheets for the medical conditions associated with OHD highlighted in this chapter that you could use in future work (e.g., share with other educators, families, etc.). Be sure to include both strengths and challenges for students with OHD. Feel free to use the resources shared in this section along with your research.