Main Body
7 Community Public Health Practice
Hector (Giovanni) Antunez
Learning Objectives
-
Identify and describe public health’s core functions and essential services
-
Describe how the core functions/essential public health services framework is operationalized in various community health assessment and improvement activities
-
Trace the development of public health practice standards over the past century
- Explain the “governmental presence in health” concept
-
Discuss how community health assessment, community health improvement planning, and organizational strategic planning serve as the pillars of modern public health practice standards and the accreditation of public health organizations.
Public Health Functions and Practice
There have been always two main questions: what are the functions of public health, and how the practice of public health looks like [in the past and today's]? As the content of this chapter develops, the questions will be answered in more detail, but in general, the functions of public health are, assessment, policy development and assurance. The practice is derived from these functions in what we know as the public health essential services. Has public health been always as it is today in the United States? The answer is no, public health has evolved over the years, and its evolution reflects how some programs have been expanded, and other better understood.
Public Health in America
In recent years, the advances made in public health has been divided in the progress made before the 1990s and after the 1990s, and the reason for this is the 1988 release of the Institute of Medicine (IOM, now, the National Academy of Medicine) document, Public Health in America, which among other things, provided a 'mission statement' and what is known as the 'substance' of public health.[1]
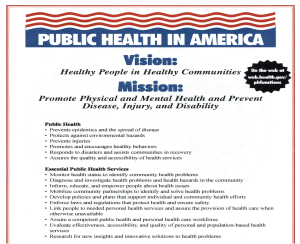 |
| Image of the original Public Health in America publication. Currently the Link to this picture is not available. The image above is from an old power point used by the author of this book. I am using the image as "Fair Use" of a public document. |
In the original document the vision and mission were clearly stated. Although, other versions of the document state the mission of public health as, "...assuring conditions in which people can be healthy," and the substance of public health as, "...organized community efforts aimed at the prevention of disease and the promotion of health."[2]
How public health looked like before 1990?
In terms of public health functions and practices, a key feature during these times included what is known as the "Basic Six" that were established before 1950, these are, vital statistics, sanitation, disease control, maternal and child health, health education and laboratory services. What does this mean? It means that most public health agencies should have these basic six as part of their public services and programs. The 1950 is used also as a crucial point in expanding the roles of public health, and it is after 1950 that the emphasis in quality control (known, as 'optimal services') became instituted. Other changes in the evolution of public health services and practices is the addition of more 'optimal services' in the 1960s and 1970s with an emphasis also in disease control.[3]
How public health looked like after 1990?
In terms of public health functions and practices, based on the IOM Public Health in America report, the Core Functions of Public Health, the Essential Public Health Services are introduced. At the same time, accreditation of public health organizations also is required and as a big step in public health for those of us who are interested in community health, the community public health practice standards became closely linked with accreditation.[4]
| Public health before 1990 | Public health after 1990 |
| Before 1950 the “Basic Six" was established | Based on the IOM Public Health in America report, the Core Functions of Public Health, and the Essential Public Health Services are introduced |
| The 1950s was a crucial point in expanding the roles of public health | Accreditation of public health organizations also is required and is a big step in public health |
| After 1950s the emphasis on quality control (known, as 'optimal services') was instituted | For those of us who are interested in community health, the community public health practice standards became closely linked with accreditation.
|
| 1988 Public Health in America (IOM) was released | |
| Table prepared by Giovanni Antunez, Licensed CC BY 4.0 |
The creation of the AGPALL and the presence of public health governance
In the middle of those two major events (before 1990 and after 1990), the formation and institution of the "Government Presence at the Local Level" (known also just as the AGPALL) appears. As the the previously mentioned Institute of Medicine (IOM-now, the National Academy of Medicine), Public Health in America report states: "The governmental public health agency has a vital function: to see to it that vital elements are in place and the mission is being adequately addressed." In simple words, the core functions of public health and the essential public health services need to have a local presence in order for the national public health programs to work. Federal guidelines are useful only if they are implemented (and applied) at the local level in the community.[5]
Although the content so far in this chapter looks very much alike to the history of public health chapter, the difference is that here, the narrative of the historical events are focused in providing information about the evolution of public health functions and practices. Can you see these differences?
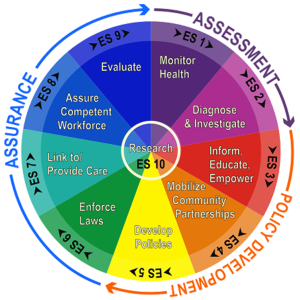
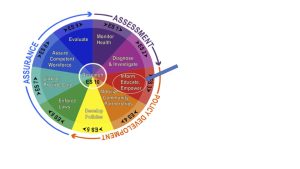
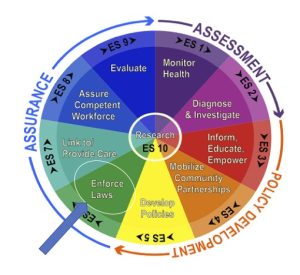
The Core functions of public health
As it has been mentioned previously, the Public Health in America IOM report clearly state the core functions of public health, these are: Assessment, Policy Development and Assurance. [6]These three elements are listed in the periphery of the following wheel that is commonly used to visualize/illustrate these concepts, see image below"
 |
| "Core Functions of Public Health" image, from CDC, Public Domain. |
Core Public Health Functions in practice [7]
In the practice, these core functions can be expressed using the following questions:
- Assessment: What should be done? This refer to the ability to take decisions based on values.
- Policy development: What will be done? How it will be done? By taking decisions based on resources and priorities.
- Assurance: How can we best do it? Taking decisions based on evidence.More specifics will be developed later in the content of these chapter, but for now, the keywords in the above content are underlined and this has been done with the intention to put an emphasis of the words that reflect specific activities that are guided by the main core public health concepts.
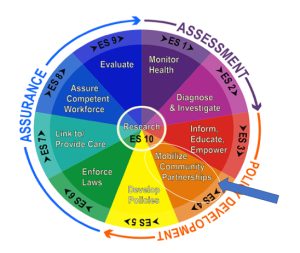
The Essential Public Health Services (EPHS)
The Essential Public Health Services (EPHS) which are contained inside the wheel have the intention to list (and explain) how each one of the core functions of public health are accomplished. In other words, what type of activities need to be done at each step in the process. [8]See image below:
 |
| "The 10 Essential Public Health Services," image, from Minnesota Dept. of Health, Public Domain. |
A list of these services are also listed below - sometimes, the numbers help to remember.
Essential Public Health Services (EPHS)
10. Research for new insights and innovative solutions to health problems.
Note: There is a new revision of this content available at the CDC Public Health Professionals Gateway Portal.[9]
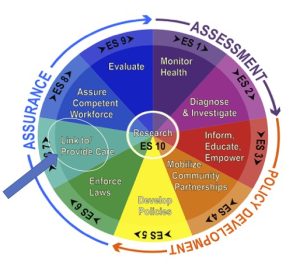
Linking both of the concepts
To operationalize (or, to integrate) the concepts, the core functions of public health are linked with the EPHS.
The first of the core public health functions: Assessment
There are two EPHS (abbreviated above as Essential Service or ES) that need to be accomplished as part of the assessment: ES 1: Monitoring health status to identify community health problems, and ES 2, Diagnosing and investigating health problem and health hazards in the community.[10],[11]
The images follow show the components of each Essential Service, and the detailed example of activities as described in the table below:
ES1 - Monitor Health
 |
| Monitor Health, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
ES2 Diagnose and Investigate
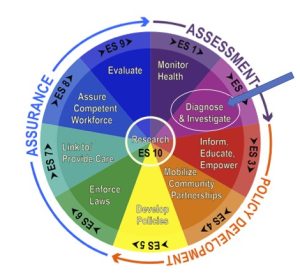 |
| Diagnose and Investigate, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
| Linking Core Functions of Public Health and EPHS | Core Functions of Public Health | Essential Public Health Service (EPHS) | Activities (How?) |
|---|---|---|---|
| Assessment | Monitoring the health status of the community | Accurate, ongoing assessment of the community’s health status | |
| Identification of threats to health | |||
| Determination of health service needs | |||
| Attention to the health needs of the groups that are higher risk than the total population | |||
| Diagnose and Investigate the health problems and health hazards in the community | Access to a public health laboratory capable of conducting rapid screening and high-volume testing | ||
| Active infectious disease epidemiology programs | |||
| Technical capacity for epidemiologic investigation of disease outbreaks. | |||
| Table prepared by Giovanni Antunez, Licensed CC BY 4.0 |
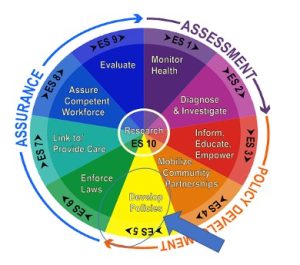
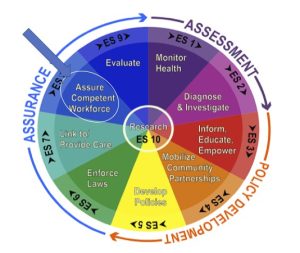
The second of the core public health functions: Policy Development
There are three EPHS (abbreviated above as Essential Service or ES) that need to be accomplished as part of the assessment: ES 3: Inform, educate, and empower people about health issues. SE 4: Mobilize community partnerships to identify and solve health problems. And, SE 5: Develop policies and plans that support individual and community health efforts. The image below visualize the entire group of essential services under policy development.
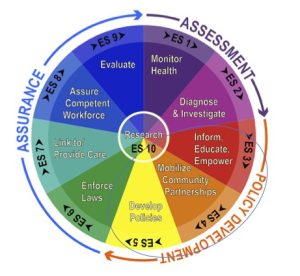 |
| Policy Development, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
To continue with the content, the images that follow show the above mentioned components for each Essential Service, and the detailed example of activities as described in the table below:
ES 3: Inform, educate, and empower people about health issues.
 |
| Inform, Educate, and Empower people about health issues, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
ES 4: Mobilizing community partnerships to identify and solve health problems
 |
| Mobilizing community partnerships to identify and solve health problems, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
ES 5: Developing policies and plans that support individual and community health
 |
| Developing policies and plans that support individual and community health, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
| Linking Core Functions of Public Health and EPHS | Core Functions of Public Health | Essential Public Health Service (EPHS or just ES) | Activities (How?) |
|---|---|---|---|
| Policy development | Inform, educate, and empower people about health issues. | Informing, educating, and empowering people about health issues | |
| Community development activities | |||
| Social marketing and targeted media public communication | |||
| Provision of accessible health information resources at community level | |||
| Active collaboration with personal healthcare providers to reinforce health promotion messages and programs | |||
| Joint health education programs with schools, churches, work sites, and others | |||
| Mobilizing community partnerships to identify and solve health problems | Convening and facilitating partnerships among groups and associations | ||
| Undertaking defining health improvement planning process and health projects | |||
| Building a coalition to draw on the full range of potential human and materials resources to improve community health | |||
| Developing policies and plans that support individual and community health | Leadership development at all levels of public health | ||
| Systematic community level and state level planning for health improvement in all jurisdictions | |||
| Table prepared by Giovanni Antunez, Licensed CC BY 4.0 |
The third of the core public health functions: Assurance
There are four EPHS (abbreviated above as Essential Service or ES) that need to be accomplished as part of the assurance core function: ES6: Enforce laws and regulations that protect health and ensure safety.
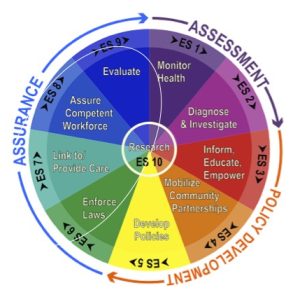 |
| Assurance of the public’s health services, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
ES 6: Enforce laws and regulations that protect health and ensure safety
 |
| Enforce laws and regulations that protect health and ensure safety, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
ES 7: Link people to needed personal health services and assure the provision of health care when otherwise unavailable.
 |
| Link people to needed personal health services and assure the provision of health care when otherwise unavailable, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
ES 8: Assure a competent public health and personal health care workforce.
 |
| Assure a competent public health and personal health care workforce, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
ES 9: Evaluate effectiveness, accessibility, and quality of personal and population-based health services.
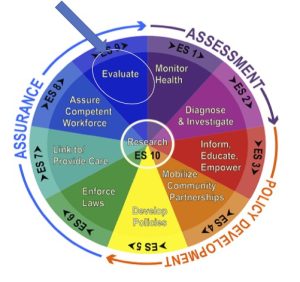 |
| Evaluate effectiveness, accessibility, and quality of personal and population-based health services, Annotation (arrow above) added by Giovanni Antunez from "Core Functions of Public Health" image, from CDC, Public Domain. |
| Linking Core Functions of Public Health and EPHS | Core Functions of Public Health | Essential Public Health Service (EPHS or just ES) | Activities (How?) |
|---|---|---|---|
| Assurance | Enforce laws and regulations that protect health and ensure safety | Enforcement of sanitary codes, especially in the food industry | |
| Protection of drinking water supplies | |||
| Enforcement of clean air standards | |||
| Animal control activities | |||
| Follow-up of hazards, preventable injuries, and exposure-related diseases identified in occupational and community settings | |||
| Monitoring quality of medical services (e.g. laboratories, nursing homes, and home healthcare providers) | |||
| Review of new drug, biologic, and medical device applications | |||
| Linking people to needed personal health services and ensuring the provision of health care | Assurance of effective entry for socially disadvantaged people into a coordinated system of health care | ||
| Culturally linguistically appropriate materials and staff to ensure linkage to services for special population groups | |||
| Ongoing care management | |||
| Transportation services | |||
| Targeted health education/promotion/disease prevention to high-risk population groups | |||
| Ensuring a competent public and personal healthcare workforce | Education, training, and assessment of personnel (including volunteers and other lay community health workers) to meet community needs for public and personal health services | ||
| Efficient process for licensure of professionals | |||
| Adoption of continuous quality improvement and lifelong learning programs | |||
| Active partnerships with professional training programs to ensure community relevant learning experiences for all students | |||
| Continuing education in management and leadership development programs for those charged with administrative/executive roles | |||
| Evaluating effectiveness, accessibility, and quality of personal and population-based health services | Assessing program effectiveness | ||
| Providing information necessary for allocating resources and reshaping programs | |||
| Researching for new insights and innovative solutions to health problems | Full continuum of innovation, ranging from practical, field-based effort to fostering change in public health practice to more academic efforts to encourage new directions in scientific research | ||
| Continuous linkage with institutions of higher learning and research | |||
| Internal capacity to mount timely epidemiologic and economic analyses and conduct health services research. | |||
| Table prepared by Giovanni Antunez, Licensed CC BY 4.0 |
Putting it all together
If we go back to where we started (look at the wheel in the image below):
- The the core functions of public health are in the periphery of the wheel.
- The Essential Public Health Services (EPHS) are contained inside the wheel.
- And, finally, the center of the wheel is Research.
 |
| "The 10 Essential Public Health Services," image, from Minnesota Dept. of Health, Public Domain. |
Putting research at the center
Putting research at the center of of the wheel is a way to show and remind the public health practitioners that there is room for research in each of the components. For example, if we take Essential Service (ES) 1 Monitor Health, a research focused on the progress made by a well-baby clinic that had introduced a new health education program for parents to learn about nutrition for their babies, the 'monitoring' of the progress made in the first three months of the program, and then, six months later can be the center of the research effort.
Linking the core functions, the EPHS and research
Using the "The 10 Essentials Public Health Services (EPHS)" wheel (Shown above), pick one core public health function and link with one or, two EPHS, then, choose a public health topic to research and develop (outline, list) the main components of the research program that you will conducted. You can start by looking at my example just above this on the Putting research at the center above.
The Community Health Needs Assessment, also known as the Community Needs Assessment - without the 'Health' word, is a process used to identify the needs of a community. It is a collaborative effort between the community health educator and other public health professionals that mobilizes the community to improve the health of its members. The assessment identifies the priorities, resources, and other elements necessary for achieving health improvement in the community. Examples can be found in websites from Local Health Departments and similar programs. [12]
Key elements of a Community Health Needs Assessment:
- Be a collaborative process
- Mobilize the community
- Develop priorities
- Gather resources
- Plan to improve the health of the community
How is a Community Health Needs Assessment (CHA) done?
First, ask yourself these questions: what do you want to know about your community? Who are they, where are they located, who lives there, what resources are available to the people who live there? And the questions continue until you decide when to stop asking more questions depending on your goals, and needs.
Secondly, it is customary to use a series of sources to conduct the assessment, the following are the most common sources of information used in this process:
1. The National Census: here you can find the general information about your community, including the demographics of your target population.
2. The county health information (for specifics about the community's health issues and resources.
3. Chamber of Commerce (for collaboration with local businesses).
4. Educational information from the Education Dept. in the area.
5. Dept. of Labor (for the report on the jobs available in the targeted community.
1. The National Census
2. The county health information
3. Chamber of Commerce
4. Education Dept.
5. Dept. of Labor
Thirdly, conduct a meeting with the community local leaders representing several areas of interest and/or work. For example, union leaders, school principals, representatives of the chamber of commerce, county jail, police dept., fire dept., local public health, clinics, and hospitals representatives, childcare representatives, and any other that you considered appropriate, or, relevant. Use the meeting to create a list of community needs (in order of priority) as perceived by the community members participating in the meeting. To do this effectively, the Delphi technique is commonly used, but independently of the format used to assess the needs, the important point is that a list of community needs is created. Once you have the list, use it to plan your program. Follow up also with those local leaders who participated in the mentioned meeting.
Write a report to disseminate the results or, to plan further
Prepare a report in which you summarize your findings from the information that you had collected, from your review of sources of information mentioned before, and also from the meetings with the community leaders. The content of the report can be used to answer the questions that you made at the beginning of the process. Use the report to inform the planning of the next step, which is the Community Health Improvement Plan.
 |
| "Example of a community health assessment" image, from Tacoma-Pierce Health Dept., no license stated. |
Learn more about the community health assessment:
The CDC has lots of information, examples, and resources available about the community health assessment.
The next step in the process is the Community Health Improvement Plan (CHIP)
 |
| Example of the cover report of a “Community Health Improvement Plan” image, from the Healthy Williamson County, no license stated. |
- Address issues from the Community Health Assessment
- Helps to Setting the priorities identified by the community
- Instead of a short term effort, it is a Long-term effort
- Promotes Broad participation of leaders and organizations in the community
 |
| "The CHIP (Community Health Improvement) Model," image fromThe Future of the Public's Health in the 21st Century, Public Domain. |
How is a Community Health Improvement Plan done?
There are several approaches to do this, but some of these approaches are highly recommended because they are user-friendly, and not that hard to implement. These approaches are theoretical frameworks that are used to guide the process, and because of their practicability, they are also known as protocols (models). The most used of all these frameworks or, protocols are:
- APEXPH (Assessment Protocol for Excellence in Public Health)
- PACE EH (Protocol for Assessing Community Excellence in Environmental Health) - is used to assist the APEXPH especially when the analyzed issue is environmental)
- Action through Planning and Partnerships (MAPP) that can be used alone or, added to the APEXPH
The following section describes the most salient (relevant) elements of these protocols.
APEXPH (Assessment Protocol for Excellence in Public Health)
This protocol (APEXPH) is considered a method for comprehensive public health planning that can be implemented by state and local health departments. It is a three-part process used by local health departments (LHD) to assess their internal capacity and to identify priority health issues existent in the community. The results of the assessment are used to develop action plans. The mentioned three parts of the APEXPH are listed as follows:
- Part 1 – Organizational Capacity Assessment
- Part 2 – The Community Process
- Part 3 – Completing the Cycle (monitoring and evaluating the organizational plan).
As it is customary for all these protocols, there are benefits and limitations of the APEXPH, these are listed in the brief table below:
| APEXPH - Benefits |
APEXPH - Limitations |
|
Assess organization and management of Local Health Dept. (LHD)
|
Local Health Dpt. (LHD) focused
|
|
Provide framework for working with community
|
Measures may be out of date
|
|
Link internal assessment with community’s priority areas
|
Part 3 not well developed
|
|
Establish the leadership role of the LHD
|
Did not provide adequate attention to Environmental Health
(To solve this issue the APEXPH can be assisted by using the PACE EH)
|
|
|
Many local health departments have limited resources for the data analysis and synthesis needed for APEXPH. |
|
"APEXH Benefits and Limitations," table prepared by Giovanni Antunez, Licensed CC BY 4.0
|
These days, the APEXPH is used in combination with the other two models, the PACE EH, and the MAPP, for this reason, the first of these two is discussed below:
PACE EH (Protocol for Assessing Community Excellence in Environmental Health) - is used to assist the APEXPH especially when the analyzed issue is environmental)
PACE EH as a community-based methodology, is used mainly for the evaluation and characterization of local environmental health conditions found in communities around the United States. As an evaluating and characterization tool, it is very useful for identifying populations at risk of environmental exposure; and prioritizing local actions, programs, and policies. How PACE EH works is by engaging the public’s involvement; collecting necessary and relevant information about community environmental health status; ranking environmental health issues; and setting local priorities for action.
PACE EH works by
- Characterizing and evaluating local environmental health conditions and concerns
- Identifying populations at risk of exposure to environmental hazards
- Identifying and collecting meaningful environmental health data
- Setting priorities for local action to address environmental health problems
- Identifying populations at risk of exposure to environmental hazards
In addition, the following diagram presents the most commonly tasks when using the PACE-EH protocol[15]:
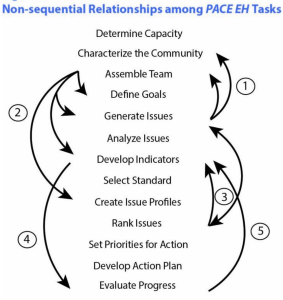 |
| "The 13 Tasks of PACE-EH," image from EPA, Public Domain. |
PACE EH has several benefits that are listed below:
| PACE EH - Benefits |
|
Greater credibility for local public health initiatives.
|
|
Assists on the creation and implementation of collaborative local environmental health improvement plans.
|
| Can be used combined with other community needs assessment tools. |
|
Focuses on environmental health issues that communities are experiencing increasing public's participation
|
PACE EH and MAPP
The following is an image presenting the major pieces [components] of the PACE-EH assessment model combined with another common model known as MAPP (Mobilizing for Action through Planning and Partnerships). [16]
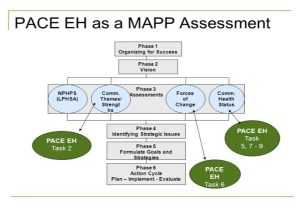 |
| "The PACE EH in combination with MAPP," image, PPT - MAPP: What, When and; Why? PowerPoint Presentation, Slide Serve. |
PACE-EH and C-FERST
The PACE-EH model can be also used with other more recent approach known as the Community-Focused Exposure and Risk Screening Tool (C-FERST). The Environmental Protection Agency - EPA CARE Program has been a key partner in developing C-FERST. Many EPA CARE communities that have received this type of grant have used the PACE-EH model (which has also a Guidebook)[17], along with the CARE Roadmap and the CARE Resource Guide, to assist with community assessment. The main reason this is highly recommended is that the C-FERST provides certain tools and pieces of information that can help the program implementation team with the tasks recommended by the PACE-EH model. [18]
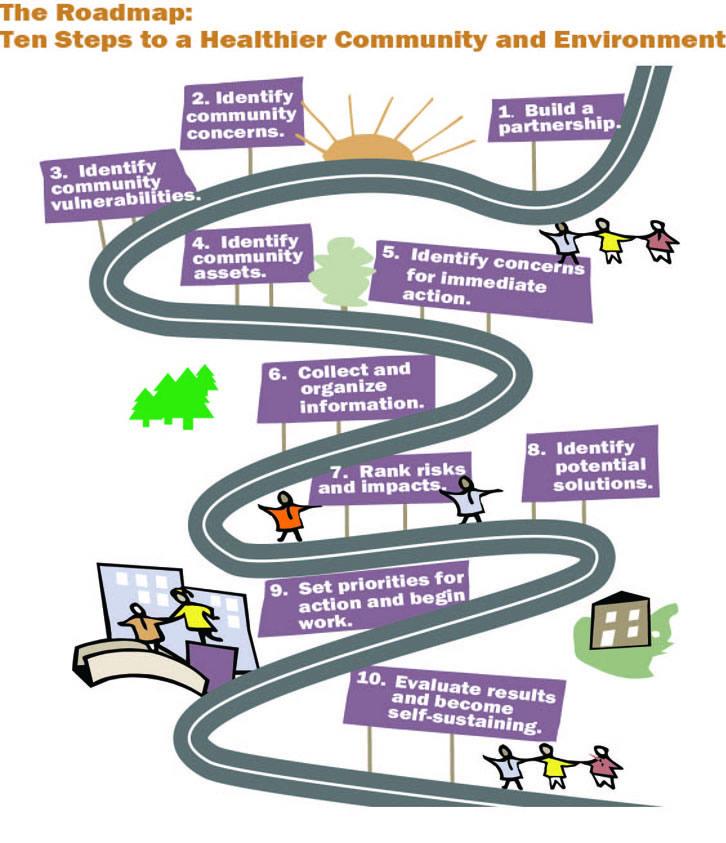 |
| “Ten Steps to a Healthy Community Environment,” image from Plan Your Project with Community Guides and C-FERST, EPA, Public Domain. |
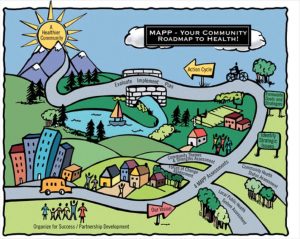
When it comes to the most common community needs assessments and public health planning models, it is important to review MAPP and how it has evolved.
What MAPP is and how it was developed
The APEXPH model evolved into MAPP (Mobilizing for Action through Planning and Partnerships), which over the years has become a very popular approach for community planning and program implementation in public health practice. The following image summarizes the major components of this model:
 |
| “MAPP”, image from the Community Tool Box, University of Kansas, Public Domain. |
| MAPP - Benefits |
|
Increases visibility of public health.
|
| Creates advocates for public health. |
| Anticipates and manages change. |
|
Creates a stronger public health infrastructure.
|
| Builds stronger partnerships. |
| Builds public health leadership. |
 |
| “Mobilizing for Action through Planning and Partnership (MAPP),” image, Sullivan County Health Department, Public Domain. |
When a comparison is made about the benefits (advantages) and disadvantages of MAPP compared with the original model, APEXH; the differences are clear that MAPP is an expanded version of its APEXH, making MAPP a highly used model for public health planning, implementation, and evaluation. See the differences below:
| Differences between APEXH and MAPP | |
|---|---|
| APEXH | MAPP |
| Build Local Health Department (LHD) leadership | Build LHD leadership, but also promote community responsibility for the health of the public |
| Assess LHD capacity for delivering public health services | Assess capacity of entire local public health system |
| Operational planning
|
Strategic planning |
| Focus on health status
|
Focus on health status, community perceptions, forces of change, and local public health system capacities |
| Develop plans to address needs
|
Strategically match needs, resources, ideas, and actions |
| "Differences between APEXH and MAPP," image/table prepared by Giovanni Antunez, Licensed CC BY 4.0
|
|
Key Takeaways
Putting it all Together
The three main pillars that guide the practice of public health in the United States are:
- Health Improvement Plan,
- Community Health Assessment, and
- The Agency Strategic Plan.
The Health Improvement Plan and Community Health Assessment have already been covered in the previous content of this chapter. The Agency's Strategic Plan is the third pillar which helps to ensure an effective and coordinated response to public health challenges.
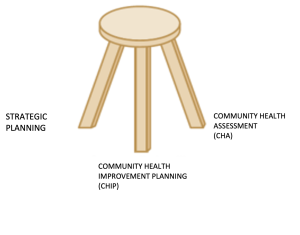 |
| "The three pillars of public health," Image prepared (modified from original image of the stool available elsewhere in the Internet, used as "Fair Use") by Giovanni Antunez, Licensed CC BY 4.0 |
Strategic planning, community health assessment, and community health improvement plans
In this context, the last part of this chapter will cover the use of strategic planning and community health assessments leading to community health improvement plans by local and state public health departments, the use of these tools has increased considerably across the nation with the need (and interest) of public health accreditation (at the professional and local/state health departments. A NACCHO 2016 report states that the participation over time in a community health assessment (CHA), community health improvement plan (CHIP), and/or strategic plan (SP) within five years increased since 2010. In 2016, more than three-quarters of LHDs had completed a CHA (78%), two-thirds had completed a CHIP (67%), and approximately half had completed an SP (53%) within the past five years. Just under half (44%) had completed all three processes within the past five years, a requirement for PHAB accreditation. [20]
In addition to the above-reported information, the level of collaboration between Local Health Departments (LHDs) and Nonprofit Hospitals on Community Health Assessments in, the United States, in 2016 also increased compared with previous years (or the baseline data used by the study/report. Below is an image representing these findings:
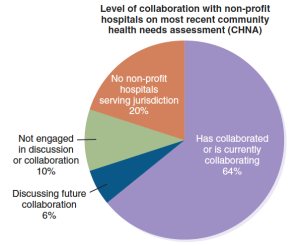 "Collaboration between Local Health Departments (LHDs) and Nonprofit Hospitals on Community Health Assessments," Image from the National Association of County and City Health Officials (NACCHO) 2016). |
In recent years, the level of collaboration between LHDs and other organizations including nonprofit hospitals has also increased with the increased access to health insurance in the U.S. population through the Affordable Care Act (also known as 'Obama Care'); more information has been needed and the Local Health Departments (LDs) had this information that has been collected through the community health needs assessments and related tools/reports.
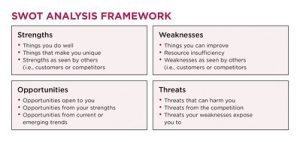
Strategic Planning
Also, with the need to increase efficiency at the Local Health Departments (LHDs), the use of the strategic planning has become a common practice, creating more and more need for training of how the strategic planning works, and what tools are available to do this. The most common tools used in the strategic planning process include: a) Identifying or, revisiting (if these already exist) the institution's or program's Values, Mission, Vision, and Strategic Priorities; b) conducting a SWOT (Strengths, Weaknesses, Opportunities and Threats) of the institution/program and; c) Layout of a General Logic Model; and other relevant information available including the Community Health Needs Assessment written report. Many of these tools can be identified in a strategic report from the New York Health Department[21] or, by searching online for other examples. Also, to visualize some of the steps of the strategic planning process, the following images are presented:
 |
| “The strategic planning process,” image from Wikimedia Commons, Licensed CC BY-SA 3.0 |
The image above captures most of the elements of the strategic planning process, especially the setting of a mission (the vision is not mentioned but it is implied), but pay attention that the word, 'strategy' is used. Additional element that is considered very useful to conduct before writing the strategic planning is the SWOT analysis, which is visually presented in the image below:
 |
| "SWOT analysis diagram," image from image from Wikimedia Commons,Licensed CC BY-SA 2.5 |
The SWOT (Strengths, Weaknesses, Opportunities and Threats) analysis can show the institution/organization/program where they are in the process by identifying especially their strengths, and opportunities if we look at the analysis positively. The following image shows in more detail (content) the SWOT process
 |
| "SWOT analysis," image, from Flicker, Licensed CC BY-NC-ND 2.0 |
And the last part of the content here is the development of a logic model that outlines and shows how the above pieces of the strategic analysis articulate (or, interact) with each one of the components used in the process. See image below:
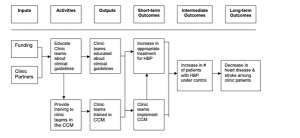 |
| “Example of Logic Model for Hypertension,” image from CDC Logic model report p 6, Public Domain. |
Key Takeaways
Public Health Department Accreditation
The concepts presented so far in this chapter, which include information about the 10 essential public health services and the core functions of public health, national standards, also on how to plan properly for public health practice using the strategic planning approach are important standards for all local health departments (state, tribal, local, and territorial). These standards can serve as a guide and measurement tool to assess their effectiveness in the state and local communities that they serve. In addition, these standards can be also used as the basis for a system of national accreditation, which helps to promote efficiency, accountability, and visibility among other things.[22]
 |
| "Public Health Accreditation Seal," image from The St. Mary’s County Health Department (SMCHD), Fair Use. |
Accreditation history and benefits
Until recent years, there was no national accreditation program for public health departments but starting in September 2011, the Public Health Accreditation Board (PHAB) has recognized health departments that meet national standards which ensures the provision of the essential public health services in their communities. As today, several public service and health-related entities—such as hospitals, schools, and universities—have accreditation programs. What are the main benefits of institutional public health accreditation? According to a NORC (National Opinion Research Center) report at the University of Chicago, Illinois, U.S., Health departments agree that accreditation helps them to the following: [23],[24]
- Stimulate quality improvement
- Improve accountability and transparency
- Improve the capacity of the department to provide high quality programs and services
- Strengthen the health department’s relationship with key partners in other sectors (e.g., healthcare, social services, education)
- Help the health department use health equity as a lens for identifying and addressing health priorities
- Increase the extent to which the health department uses evidence-based practices
- Strengthen the utilization of resources
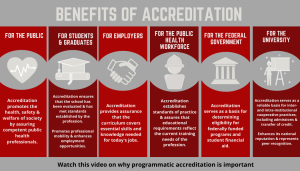 |
| "The benefits of Accreditation", image from CEPH, used as Fair Use because no license is stated. |
How the idea of Public Health Accreditation was Born
Accreditation came initially as a recommendation of the Academy of Medicine (known before as the Institute of Medicine-IOM) The Future of Public Health in the 21st Century report, which mentioned that local and state health departments seek accreditation to improve the quality of their services. The idea was supported also by the Centers for Disease and Prevention (CDC), the Robert Wood Johnson Foundation, and other directly related organizations including the American Public Health Association (APHA), the National Association of County Health Departments (NACCHO), and similar. As part of the initiative, the Public Health Accreditation Board (PHAB) was created as an independent non-profit organization that carries out the original recommendations. After years of work, the PHAB produced the standards needed for accreditation which requires that all public health agencies seeking accreditation must complete within the last five years, a strategic plan, a community health needs assessment (CHA), and the Community Health Improvement Plan (CHIP) before submitting an accreditation application. Once the application is submitted, the public health department needs to respond to a questionnaire that contains a series of questions in the 12 domains made up of the 10 Essential Public Health Services. Also, two additional domains are governance and administration and management.[25],[26]
What are the domains of public health agencies' accreditation? The following are the main domains:
Public Health Accreditation Domains (or the PHAB = Public Health Accreditation Board Domains)[27] |
| Conduct assessment activities focused on population health status and health issues facing the community. |
| Investigate health problems and environmental public health hazards to protect the community. |
| Inform and educate about public health issues and functions. |
| Engage with the community to identify and address health problems. |
| Develop public health policies and plans. |
| Enforce public health laws and regulations. |
| Promote strategies to improve access to health care services. |
| Maintain a competent public health workforce. |
| Evaluate and continuously improve processes, programs, and interventions. |
| Contribute to and apply the evidence base of public health. |
| Maintain administrative and management capacity. |
| Build a strong and effective relationship with governing entity. |
|
Note: the list of domains above has been taken directly from the article cited in the title above. |
Some statistics reported in recent years have provided information about the number of public health agencies that have achieved accreditation - these numbers can. be found in several online resources but mainly on the Public Health Accreditation Board (PHAB) website. [28]
Chapter conclusion: the content in this chapter centered on the topic of Community Public Health Practice in the United States. The main topics covered include the history of public health in the United States, the core functions of public health, the ten (10) essentials of public health services, the development of community health assessments, community health improvement plans, strategic planning, and related tools, and also accreditation in the public health services agencies in the United States.
- Institute of Medicine (1988). The Future of Public Health. 2, A Vision of Public Health in America: An Attainable Ideal. From the Committee for the Study of the Future of Public Health. Washington (DC): National Academies Press. From https://www.ncbi.nlm.nih.gov/books/NBK218220/ ↵
- Institute of Medicine (IOM). (2003). Chapter 2, History and Current Status of Public Health Education in the United States, In the eBook by Gebbie K, Rosenstock L, Hernandez LM, editors. Who Will Keep the Public Healthy? Educating Public Health Professionals for the 21st Century. Washington (DC): National Academies Press (US). From: https://www.ncbi.nlm.nih.gov/books/NBK221176/ ↵
- Institute of Medicine (IOM). (2012). The Future of the Public's Health in the 21st Century. Preface. Committee on Assuring the Health of the Public in the 21st Century. Washington (DC): National Academies Press (US. From https://www.ncbi.nlm.nih.gov/books/NBK221223/ ↵
- The content of public health before 1990 and after 1990 share the same reference: Institute of Medicine (IOM). (2012). The Future of the Public's Health in the 21st Century. Preface. Committee on Assuring the Health of the Public in the 21st Century. Washington (DC): National Academies Press (US. From https://www.ncbi.nlm.nih.gov/books/NBK221223/ ↵
- Carlson, V., Chilton, M. J., Corso, L. C., & Beitsch, L. M. (2015). Defining the functions of public health governance. American journal of public health, 105 Suppl 2(Suppl 2), S159–S166. https://doi.org/10.2105/AJPH.2014.302198 ↵
- Los Angeles County Department of Public Health. (n.d.). The Core Functions [of Public Health]. From http://publichealth.lacounty.gov/qiap/docs/CoreFunctions.pdf ↵
- Centers for Disease Control and Prevention. (n.d.). The core functions of public health In “Public Health Professionals Gateway.” From https://www.cdc.gov/publichealthgateway/ ↵
- Centers for Disease Control and Prevention. (n.d.). 10 Essential Public Health Services. From https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html ↵
- Centers for Disease Control and Prevention. (n.d.). 10 Essential Public Health Services. From https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html ↵
- These and the rest of the content that follows came from the major following source of information: Centers for Disease Control and Prevention. (n.d.). Original Essential Public Health Services Framework. From https://www.cdc.gov/publichealthgateway/publichealthservices/originalessentialhealthservices.html ↵
- The following information has been used also to prepare the content about the essential public health services: Public Health National Center for Innovation (PHNCI), recently renamed to PHBA. (n.d.). The 10 Essential Public Health Services. From https://phaboard.org/center-for-innovation/public-health-frameworks/the-10-essential-public-health-services/ ↵
- McLean County Health Department. (n.d.) Community Health Needs Assessment & Health Plans. Bloomington, Illinois. From https://www.mcleancountyil.gov/1656/Community-Health-Needs-Assessment-Health ↵
- CDC. (no date). Community Health Assessment & Health Improvement Planning. From https://www.cdc.gov/publichealthgateway/cha/index.html ↵
- Institute of Medicine (IOM). (2002). The CHIP (Community Health Improvement) model, B, Models for Collaborative Planning in Communities in The Future of the Public's Health in the 21st Century. National Academies Press (US), Washington (DC). From https://www.ncbi.nlm.nih.gov/books/NBK221247/ ↵
- United States Environmental Protection Agency (EPA). The 13 Tasks of PACE-EH. From https://19january2017snapshot.epa.gov/c-ferst/use-c-ferst-protocol-assessing-community-excellence-environmental-health_.html ↵
- Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. (2002). B, Models for Collaborative Planning in Communities in The Future of the Public's Health in the 21st Century. National Academies Press (US), Washington (DC). From: https://www.ncbi.nlm.nih.gov/books/NBK221247/ ↵
- United States Environmental Protection Agency (EPA). Use C-FERST with the Protocol for Assessing Community Excellence in Environmental Health. What is the PACE-EH Guidebook? From https://19january2017snapshot.epa.gov/c-ferst/use-c-ferst-protocol-assessing-community-excellence-environmental-health_.html ↵
- United States Environmental Protection Agency. (n.d.). Community-Focused Exposure and Risk Screening Tool (C-FERST). From https://19january2017snapshot.epa.gov/c-ferst_.html ↵
- University of Kansas. Community Toolbox. (n.d.). Section 13. MAPP: Mobilizing for Action through Planning and Partnerships. From https://ctb.ku.edu/en/table-of-contents/overview/models-for-community-health-and-development/mapp/main ↵
- National Association of County and City Health Officials (NACCHO). (2016). National Profile of Local Health Departments, Chapter 9: Assessment, Planning, and Accreditation. Washington, DC: National Association of County and City Health Officials; 2017. From http://nacchoprofilestudy.org/reportspublications/ ↵
- New York State Department of Health. (2018). Strategic Plan. Available at https://www.health.ny.gov/commissioner/docs/strategic_plan_2018-2023.pdf. ↵
- Leider, JP., Kronstadt, J., Yeager, VA., Hall, K., Saari, CK., Alford, A., Tremmel Freeman, L., Kuehnert, P. (2021). Application for Public Health Accreditation Among US Local Health Departments in 2013 to 2019: Impact of Service and Activity Mix American Journal of Public Health 111, 301_308. From https://doi.org/10.2105/AJPH.2020.306007 ↵
- CDC. (n.d.). Benefits & Impacts of Accreditation, from https://www.cdc.gov/publichealthgateway/accreditation/benefits.html ↵
- Siegfried, A., Heffernan, M., Melnick, M., Papanikolaou, M. (NORC Evaluation Team). (2019). Assessing Outcomes from Public Health Accreditation. From https://phaboard.org/wp-content/uploads/NORC-Evaluation-Slides.pdf ↵
- Riley, W. J., Bender, K., & Lownik, E. (2012). Public health department accreditation implementation: transforming public health department performance. American journal of public health, 102(2), 237–242. https://doi.org/10.2105/AJPH.2011.300375 ↵
- PHAB. (n.d.). The Public Health Accreditation Board (PHAB). From https://phaboard.org/about/ ↵
- Riley, W. J., Bender, K., & Lownik, E. (2012). Public health department accreditation implementation: transforming public health department performance. American journal of public health, 102(2), 237–242. https://doi.org/10.2105/AJPH.2011.300375 ↵
- PHAB. (n.d.). The Public Health Accreditation Board (PHAB). From https://phaboard.org/ ↵
EPHS refers to those services considered essential (the basic and necessary).
A community health needs assessment is a collaborative process between the community health educator, or, any other public health professional that is used to mobilize the community by identifying the needs of this community, what are the priorities, resources, and other related elements that can be used to improve the health of the people in the community.
the group for whom the program intends to be provided, or, the population for which the intervention is designed.
It is a method of group decision-making and forecasting that involves successively collating the judgments of experts.
A community health improvement plan is a long-term, systematic effort to address public health problems based on the results of community health assessment activities and the community health improvement process. (taken from the CDC website at https://www.cdc.gov/publichealthgateway/cha/index.html
Strategic planning is a process in which an organization's leaders define their vision for the future and identify their organization's goals and objectives. It is a common method used to improve the efficiency and accountability of an organization or program.
