Main Body
11 Public health work during emergencies including pandemics
Hector (Giovanni) Antunez
Learning Objectives
By the end of this chapter, the learner will be able to
-
Learn about the role of public health during emergencies and disasters including epidemics and pandemics
- Define the major terms, emergency, disaster, recovery, epidemics, pandemics, endemic and related terminology
- List the major types of emergencies and how its classification is useful for planning and proper response
- Describe the series of public health activities during emergencies including pandemics
- Recognize the importance of collaboration among inter-agencies and public health, including the community resources during emergencies including pandemics
- Recognize the importance of proper public health leadership during emergencies including pandemics
- Identify the series of public health preparations required to be ready for emergencies including pandemics
- Provide a series of case studies and examples of proper response during emergencies including pandemics
- Consider this:
IDENTIFY the indicators, signs and symptoms for exposure to critical biological, chemical and radiological agents (BCR) (category A, B, C), blast injuries and trauma.
Although there are so many books, websites and other sources of information about emergency preparedness and disaster response, there is no complete public health book without at least the basics on this topic. To help with the vocabulary or terminology commonly used in this area of public health, the first part of this chapter will be dedicated to clarifying the terms.
 |
| “An Emergency Medical Technician, arrives during an emergency,” image from Wikipedia, Licensed CC BY-SA 3.0 |
What is an emergency?
An emergency is an urgent, unexpected, and usually dangerous situation that poses an immediate risk to health, life, property, or environment and requires immediate action.[1]
What is emergency preparedness?
It is accepted that in general, that ‘preparedness’ is a set of actions that are taken as precautionary measures in the face of potential disasters. Being prepared helps in achieving goals and in avoiding and mitigating negative outcomes.[2]
If we put together both definitions, it can be said that Emergency Preparedness is the actions and measures to prepare before an urgent situation or emergency happen.
Frequently, the word, ‘disaster’ is used as an equivalent to ’emergency,’ but are all emergencies disasters? Probably when people use any of the terms, they are referring to the same type of events. The important point, is that people take action and prepare before an emergency or disaster.[3]. As the content of the chapter progresses, the definition of disaster will expand in order to respond to the technicalities of the topic. But for now, let’s see what makes an emergency and emergency.
What makes an emergency an emergency?
It is accepted that for an incident, to be an emergency, one or more of the following must be in place:
- The event poses an immediate threat to life, health, property, or environment
- The event has already caused loss of life, health detriments, property damage, or environmental damage
- The event has a high probability of escalating to cause immediate danger to life, health, property, or environment. [4]
Public health and Emergencies
Independently of the type of emergency that happens, the unexpected event becomes also a public health situation. There is always life and health endangered and also there is always the risk of disease outbreaks.
| “What is the difference between emergencies and disasters?,” Video from Albearta California, Fair Use. |
Emergencies and Disasters
What are disasters? Disasters are serious disruptions to the functioning of a community that exceed its capacity to cope using its own resources. Disasters can be caused by natural, man-made and technological hazards, as well as various factors that influence the exposure and vulnerability of a community.[5]
A definition of “disaster” by the Federal Emergency Management Agency (FEMA)
Classification of Disasters
In a simple manner, disasters can be classified into two categories, natural and man/woman-made. Natural disasters are those caused by nature, examples include winter storms, flooding, heat emergencies, utility disruption, hurricanes, earthquakes, tsunamis, etc. And, man/woman-made disasters which are provoked by humans, examples of those include transportation accidents, fires, and terrorism.
The D-I-S-A-S-T-E-R Paradigm
Although there are so many ways in which the concept of disaster can be approached, a useful approach is to see disaster as a paradigm.Paradigm, which can be easily described as the following:
| D | Detection |
| I |
Incident Command
|
| S | Scene Security and Safety |
| A | Assess Hazards |
| S |
Support
|
| T |
Triage and Treatment
|
| E | Evacuation |
| R | Recovery |
The “D-I-S-A-S-T-E-R” paradigm developed for the NDLS Family of Courses is a mnemonic that satisfies many of these requirements, such as: a common set of definitions, a common triage model, a common organizational plan, and a simple method of classification.[7]
Each of the letters in “DISASTER” applies to a specific element of MCI recognition and response. “D” stands for “detection”, “I” for “incident command”, “S” for “scene security and safety”, “A” for “assess hazards”, “S” for “support”, “T” for “triage and treatment”, “E” for “evacuation” and “R” for “recovery”. [8] The following table provides a more detail information of the “DISASTER” paradigm components.[9]
| General Action | Question | |
| D | Detection |
Do I Detect something? What caused this?
|
| I |
Incident Command
|
Do I need Incident command? Where?
|
| S | Scene Security and Safety |
Is a Safety or security issue present?
|
| A | Assess Hazards |
Did I Assess the hazards that could be here?
|
| S |
Support
|
What Support, people, supplies are needed?
|
| T |
Triage and Treatment
|
Do I need to Triage? How much treatment is needed?
|
| E | Evacuation |
Can I Evacuate and/or transport the victims?
|
| R | Recovery | What Recovery issues are present? |
How to manage communication using this system?
To manage communications under the d-i-s-a-s-t-e-r paradigm, the following needs to be done:
- Learn a system that assures effective communication among agencies
- Use a system that promotes team work because no single organization can handle a disaster of any scale alone
- Use the ICS (Incident Command System), which is a model tool for command, control, and response coordination
ICS (Incident Command System)
For this reason, in an emergency, you are required to function in an ICS environment. Working for someone other than your day-to-day supervisor
Major components of the Incident Command System (ICS)
 |
| “The Five Components of the Incident Command System,” Image from FEMA training, Public Domain. |
In an abbreviated content, the following are the major steps to implement the Incident Command System (ICS):[11]
- The Incident Commander – Establishes command and the Incident Command Post or ICP
- The ICS controls personnel and equipment resources
- The ICS establish and maintain an effective liaison with outside agencies and organizations, including the Emergency Operations Center or EOC
Additional responsibilities of the ICS:
If needed, the Incident Commander will base the decision to expand/contract the ICS organization on 3 major incident priorities:[12]
- Life safety. The Incident Commander’s first priority is always the life safety of the emergency responders and the public.
- Incident stability. The Incident Commander is responsible for determining the strategy that will:
- Minimize the effect that the incident may have on the surrounding area.
- Maximize the response effort while using resources efficiently
- Property conservation. The Incident Commander is responsible for minimizing damage to property while achieving the incident objectives.
The Planning Section of the Incident Command System (ICS)
The Planning Section is only established during large incidents. Its responsibilities include collection, evaluation, dissemination, and use of information about the development of the incident and status of resources. Also, the creation of the Incident Action Plan (IAP), which defines the response activities and resource utilization for a specified time period.[13]
The Incident Command System Operations Section
 |
| “Safety Priorities of the Operations Section,” Image from the AMD/NDLS Manual, p17. |
The Operations section chief is responsible of directing and coordinating all operations described in the Incident Action Plan or IAP. In addition, the operations section have the following responsibilities:
- Assist the Incident Commander in developing response goals and objectives for the incident
- Request (or release) resources through the Incident Commander
- Keep the Incident Commander informed of situation and resource status within operation
The Logistics Section of the Incident Command System
The logistic section provides the facilities, services, and materials, including personnel to operate the requested equipment for the incident. This section takes on great significance in long-term or extended operations because its major functions are geared to support the incident responders. For example, the Medical Unit in the Logistics Section provides care for the incident responders not civilian victims.[14]
The Incidence Command System Finance/Administration Section
The finance/administration section is critical for tracking incident costs and reimbursement accounting. It is especially important when the incident is of a magnitude that may result in a Presidential Declaration. There is an additional characteristics of this section and it is that its functional areas can be expanded (or contracted) into additional organizational units depending of the needs to respond to the incident.[15]
What happens at the Incident Command when the needs of the incident grow?
As incidents grow, the Incident Command needs to delegate functions creating the following officers:[16]
 |
| The Officers in the Incident Command, Modified image. Looking at only one piece the image used above about ICS system. Original image from FEMA training, Public Domain. |
- The Incident Officer (IO) – this person handles all media inquiries and coordinates the release of information to the media
- The Services Officer (SO), who monitors/develops safety conditions for ensuring the safety of all assigned personnel
- The Liaison Officer (LO) who is the on-scene contact for other agencies assigned to the incident.
Remark: to emphasize about the chain of command and how it works in an Incident Command System (ICS), the following image is presented below.[17]
 |
| “The Chain of Command,” Image from FEMA Lesson 2, Public Domain. |
Are there any additional components of the Incident Command System (ICS)?
The answer to the question above is yes, there are eight common components in all ICS structure which makes the system unique, these components include a Common terminology, A modular organization, an Integrated communications, a Unity of command, a unified command structure, Consolidated IAPs, a manageable span of control, Designated incident facilities, and Comprehensive resource management.
Among these above mentioned element, a key concept of the ICS is the concept of Unified Command which includes the Incident command itself, the jurisdiction having the incident and, the liaison. The main roles and benefits of the unified command follow:[18]
 |
| “Unified Command”, image from FEMA, Public Domain |
- Provides broad-based input for decision making
- Jointly determine objectives, strategies and priorities
- Jointly select the IC and operations chief
The Unified Command is very important when for example the incident had involved multiple agencies (e.g. the fire department, the law enforcement team and the local hospital) and have to work on an incident that had affected more than one political jurisdiction.
 |
| This illustration shows three responsible agencies managing an incident together under a Unified Command”, image from FEMA, Public Domain |
Having a unified command assures that among other things, the levels of communication and operation system are coordinated in an efficient manner under a sole unified command. This makes the process more efficient and also effective. When no one jurisdiction, agency, or organization has primary authority and/or the resources to manage an incident on its own, Unified Command may be established. There is no one “Commander.” The Unified Command can allocate resources regardless of ownership or location.
As a form of summary about the Incident Command System (ICS), it can be said that as ICS has become increasingly accepted as an effective and practical tool for responding to incidents such as disasters and other types of emergencies, the concepts of ICS has become standards as part of the training in the topic of emergency preparedness and disaster response.
The next level of to talk about the role and work of local public health agencies in response to public health emergencies.
Local Public Health agencies (LPHAs) role during Emergencies
As all public health is local, Public health agencies work at the local level in case of emergencies is a collaborative effort with other “first responders,”first responders.
 |
| “First responders at the scene of a traffic accident in Hong Kong,” Image from Wikimedia, Licensed CC BY-SA 3.0 |
First responders typically include police officers (law enforcement officers), fire service members (such as firefighters, search and rescue members, technical/heavy rescue members, etc., emergency medical services members (such as EMTs or paramedics). Depending of the regulations in some jurisdictions, emergency department personnel such as doctors and nurses, who are also require to respond to some critical situations such as disasters and emergencies (in this case, these group of professional act also as first responders). In addition, in other jurisdictions, military and security forces can be authorized to act as first responders, especially the national guard.[19] The list can continue and can be more specific but only these main categories of first responders have been mentioned here for reasons of brevity. [20]
Although jurisdictions may have different regulations depending of the state, Local Public Health Agencies (LDAs) always have the responsibility to work with the first responders and the rest of the organizations that are activated when there is a health related emergency, not only for reasons of injuries, deaths, and exposure to hazardous materials, but also for the need to collect and report data to the state and national level as part of the public health efforts. Public health agencies have tremendous responsibility for dealing with emergencies in practically all states.
In general first responders are the ones who respond to the emergency and deal with the emergency more directly, while the public health agency acts as a partner with those first responders. It is accepted that in general during emergencies most LHAs (also called, Local Health Departments -LHDs) are somewhat less likely to be directly involved in emergency response; including the provisions LHAs operate laboratory services. However, the LHAs personnel [especially those in charge of the emergency department need to be vigilant and ready during emergencies]. In other words, LHAs dependent greatly in the work and reports provided by the first responders who are working directly with the emergency. One example of this is the case of the fire department which in many cases is the organization providing the delivery of services many times in coordination with the agency/department of environmental health services.
 |
| “Homeland Security Advisory System color chart”, Image from Wikimedia, Licensed Public Domain
Colors: Green: low risk. Blue: general (guarded) risk. Yellow: significant (elevated). Orange: high risk. Red Severe risk |
Besides these mentioned limitations of Local Health Agencies (LHAs), the level of readiness among LHAs has increased significantly since the year after the attacks of September 11, 2001, especially after the bioterrorism attacks with contaminated anthrax letters and packages, which called for a more active role of the public health agencies in the country. In recent years, more and more training in emergency preparedness and disaster response has been provided for public health workers, and a great number of LHAs have completed a readiness planning. It is important to note that LHAs have contributed greatly to the development of the national threat advisory system and guidelines that used in transit facilities and especially in state and national airport security systems. Now, the mentioned system is very much the standard.[21]
The training of public health workers on Emergency Preparedness and Disaster Response
Overview
The Public Health Preparedness and Response Core Competencies were created to establish a common performance goal for the public health preparedness workforce. This goal is defined as the ability to proficiently perform assigned prevention, preparedness, response, and recovery role(s) in accordance with established national, state, and local health security and public health policies, laws, and systems. To meet this goal, a series of competencies has been developed. There are several sources of information that provide the list of competencies required for public health workers in their training for emergency preparedness and disaster response. One of those sources is found at the Public Health Foundation website[22] these mentioned competencies contain four domains that are critical to build and sustain the capacity of public health workers to fulfill their responsibilities, and they listed in detail in the table below.
| Public Health Preparedness and Response Core Competencies |
1. Model Leadership
|
2. Communicate and Model Information
|
3. Plan for and Improve Practice
|
4. Protect Worker Health and Safety
|
| Source of the information: Public Health Foundation. Public Health Preparedness and Response Core Competencies. |
Once the major competencies are put into place, the next level is, where to find funding to training the public health workforce on emergency preparedness and disaster response? The answer to this question is, the funding for this type of training comes mainly from state and local preparedness grants.
Funding sources to train public health workers in emergency preparedness
After the September 11 attacks in New York, United States, which also followed several intents and perpetration of terrorism attacks, the US federal government (through the department of Homeland Security) realized that public health workers also constitute another frontline group for defense against terrorism and also for the management of emergencies and disasters, funding became allocated through a grant system. [23],[24]The funds from these grants provided billions of dollars beginning in 2002 with reductions to this funding in 2010. The funding during those years provided the opportunity for the public health system to reinforce its infrastructure and enhance quality of services provided by public health agencies at all levels (federal, state and local levels).
The CDC Emergency Preparedness Capabilities
CDC developed and implemented a system that defines public health capabilities to assist public health agencies with their strategic planning. As part of this planning, the capacity of the public health agencies to respond and prepare for emergencies was identified, including the gaps in the areas of preparedness, especially the role of jurisdictions during a response and also sustaining capabilities. In this context, the CDC created a system composed of 15 public health preparedness capabilities and its respective domains. This system become the basis for state and local public health preparedness. The system is organized in domains that have their respective tiers, this information is presented as follow.[25]
| The CDC 15 public health preparedness capabilities and its respective domains. |
|
| Domain | Capability and Tier |
| 1. Community Resilience* | Community Preparedness (Tier 1) |
| Community Recovery (Tier 2) | |
| 2. Incident Management | Emergency Operations Coordination (Tier 1) |
| Emergency Public Information and Warning (Tier 1) | |
| 3. Information Management* | Information Sharing (Tier 1)* |
| Medical Countermeasure Dispensing and Administration (Tier 1) | |
| Medical Materiel Management and Distribution (Tier 1) | |
| 4. Countermeasures and Mitigation* | Nonpharmaceutical Interventions (Tier 2) |
| Responder Safety and Health (Tier 1) | |
| Fatality Management (Tier 2) | |
| Mass Care (Tier 2) | |
| 5. Surge Management | Medical Surge (Tier 2) |
| Volunteer Management (Tier 2) | |
| Public Health Laboratory Testing (Tier 1) | |
| 6. Biosurveillance* | Public Health Surveillance and Epidemiological Investigation (Tier 1) |
| Content modified from the CDC Public Health Emergency Preparedness and Response Capabilities System. Note: The domains/capabilities with the asterisk (*) are those strongly recommended for demonstration by the committee who developed the system. | |
As seen above, ea ch capability includes a definition of the capability and a list of the associated functions, performance measures, tasks, and resources. All of this information that can be used in the planning and implementation of public health emergency preparedness programs.
Using the CDC Public Health Emergency Preparedness and Response Capabilities System
The basic recommendation to use and implement this system is that each jurisdiction determine what order of capabilities are needed in their area of work based on their jurisdictional risk assessment. This step of selecting the order of capabilities followed by the respective jurisdiction needs to be completed as part of the community preparedness capability in which the public health agency is located. To be sure that the system will be used by the jurisdiction, there are a series of capabilities that are strongly recommended for demonstration, these are the biosurveillance, community resilience, countermeasures and mitigation, incident management, and information sharing domains. Also, it is expected that the respective public health agency will use the system to assist with preparedness planning. The following image shows some of the suggested steps in the planning process.
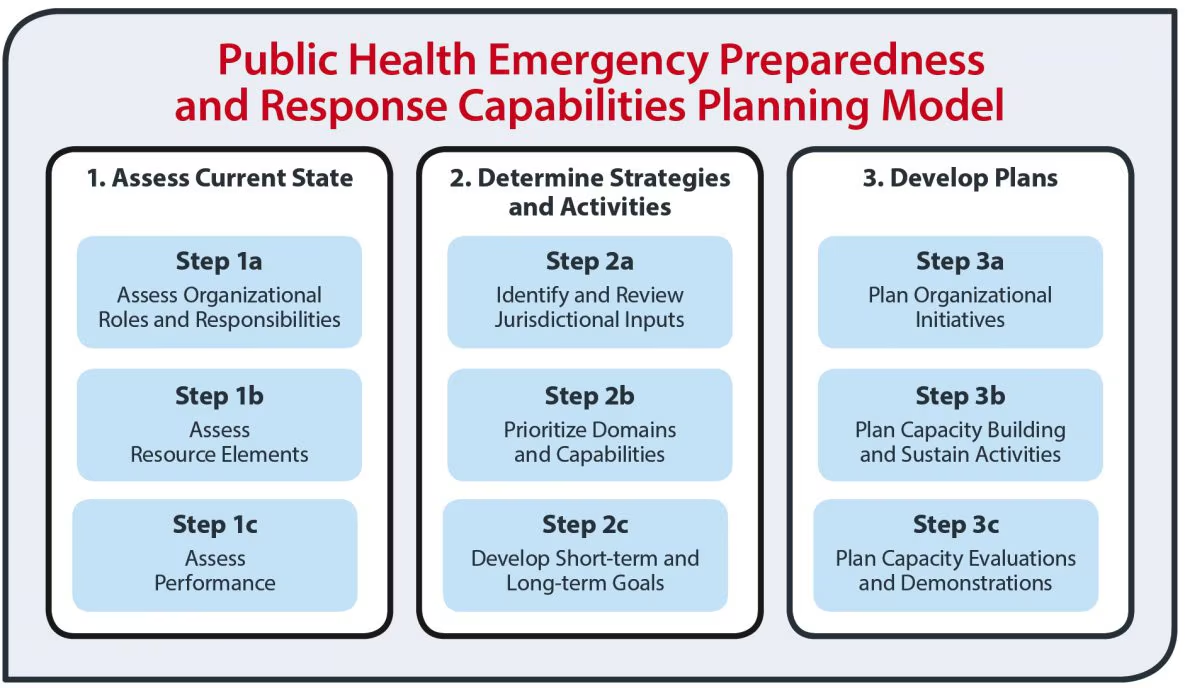 |
| “Public Health Emergency Preparedness and Response Capabilities Planning Model,” image from CDC, Licensed Public Domain |
The system is the result of the hard work of CDC, which to develop the system consulted several sources such as the DHS Target Capabilities List, some areas of content of the Pandemic and All-Hazards Preparedness Act (PAHPA), and capabilities from the National Security Strategy (NHSS). Looking at the mentioned consulted sources, it is important to note that each source provided a rich baseline body of information, for example, several of the recommendations and content for the public health preparedness capabilities system based on the PAHPA emphasis of the need to maintain consistency with other national programs. Consulting with the DHS was very useful too because the DHL capabilities list is a major component of the DHS National Preparedness Guidelines. Also, the aligning with the National Preparedness Guidelines, the CDC determined that the public health preparedness capabilities needed to be aligned with the framework of the Health and Human Services (HHS) essential public health services.
When looking into more detail inside the public health preparedness capabilities, it can be seen that each one of these capabilities identifies priority resource elements that are relevant to the daily public health routine and to the work of public health agencies with the provision of essential public health services. Although it is important that public health agencies provide emergency preparedness training to their personnel by conducting exercises, planned events and also real incidents; it is highly recommended that jurisdictions use daily public health activities to demonstrate, implement and evaluate their public health preparedness capabilities. So, the work with these capabilities become part of the nature of public health workers.
In one hand, it is important to note that the creation and use of the public health preparedness capabilities is evidence-based information, applicable preparedness literature, and a collection of experiences from experts and subject matter individuals who have been working on these issues for a long time across the federal government and the state and local public health system.
Why training of public health workers in Emergency Preparedness and Disaster Response?
One of the main reasons for the training of public health workers on the topic of emergency preparedness have been two significant events in the life of the United States, the 09/11 or September 11, 2001, which is followed by bioterrorist attacks with anthrax; and the COVID-19 pandemic. Both of the mentioned events had changed the face of public health training and also the training on emergencies and disaster response for professionals beyond the field of public health.
The concept of Weapons of Mass Destruction (WMD)
There are at list four categories of Weapons of Mass Destruction (WMD): biological, chemical and radiological and nuclear agents. The ‘nuclear’ agents would not be covered in much detail in this chapter due to the extensive amount of content that requires to just cover the most common types of WMD mentioned above. The topic of WMD became mostly known after the September 11 Terrorist Attacks in 2001. An additional event that also raised awareness and concerns is when it was reported that Weapons of Mass Destruction (WMD) existed in Iraq, and then, a war was declared on Iraq, having soldiers and army personnel also to the possibility of exposure to substances and materials that can kill, cause disease or contribute to permanent disability.
The case of Bioterrorism as an emergency
The topic of a biological attack or bioterrorism as part of the public health emergency scenarios represent a challenge, not only because of the great amount of information that needs to be known, and available but also because of the implications of response and recovery from this type of threat.
The Centers for Disease Prevention and Control (CDC) defines Bioterrorism as the intentional release or threat of release of biologic agents (i.e. viruses, bacteria, fungi or their toxins) in order to cause disease or death among human population or food crops and livestock to terrorize a civilian population or manipulate the government.[26].
Bioterrorism: most common biological agents
There are three types of biological agents that can be used for terrorism to attack a population. These agents are summarized in the table below.
| Bacterial Agents | Viruses | Biological Toxins |
| Anthrax
Brucellosis Cholera Plague, Pneumonic Tularemia Q Fever |
Smallpox
Viral Equine Encephalitis (VEE) Viral Hemorrhagic Fevers (VHF) -Ebola |
Botulinum
Staphyloccocus Enterotoxina-B Ricin T-2 Mycotoxins |
Although there are several agents listed in the table above, the most common biological agents that have been used or have the potential to be used in a bioterrorist attack include anthrax, smallpox, plague, tularemia, botulism, flavoviruses such as Marborg and Ebola. That said, it is very useful that before each one of these agents are discussed in detail, the most common routes of transmission are also reviewed. This information is presented in the following table.
| Route | Delivery method |
| Respiratory (Inhalation) | Inhalation
□Inhalation of droplets, aerosols or spores
□Agent must be dispersed as an aerosol to be effective
□1-5 μ (micron) is the ideal size of the droplet
|
| Gastrointestinal (Oral) | Food
□Food is a potentially significant route of delivery
□Secondary to either purposeful or accidental exposure to aerosol
|
| Water
□The degree of contamination depends on the dilution factor
Water contamination is a common public fear because it has the capacity to affect large numbers of people, however: □Water treatment may be effective in removal of agents
|
|
| Skin (Dermal) | Infection agents could enter by the skin through:
□Skin cuts
□Skin abrasion
□Mucosal membranes
|
Some clues that there is a possibility terrorist attacks using Weapons of Mass Destruction (WMDs)
It is important to note that there are some epidemiological clues of the presence of biological agents as Weapons of Mass Destruction (WMDs) may include the following.
- An infection appears in a non-endemic region
- An epidemic develops with morbidity and mortality rate
- Multiple simultaneous outbreaks
- Sick or dead animals of multiples types appear in a region
- When a biological agent is confirmed by the specialized laboratory, the health care personnel need to be informed about the agent ( forms of transmission, infectious properties, symptoms/ signs, treatment/control). And, management protocols should be in place
Anthrax
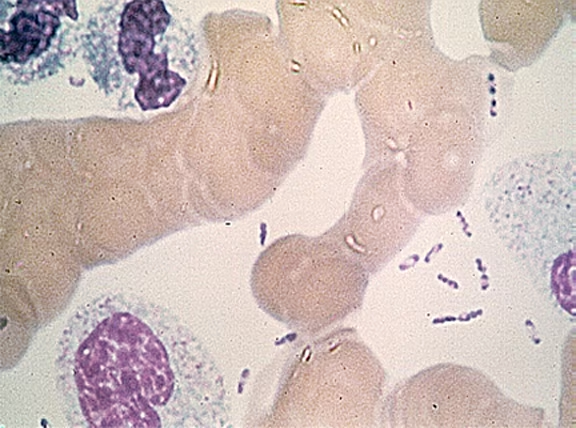
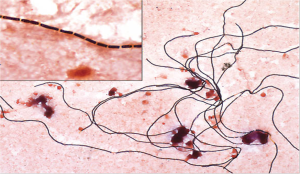 |
|
“Gram Stain of Blood in Culture Media,” image from JAMA article, Fair Use. [27] Note: Microscopic picture showing the Bacillus anthracis: Gram + bacilli in long chains. |
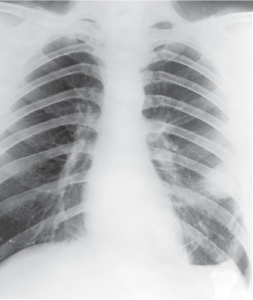
Pulmonary Anthrax
The anthrax pulmonary infection (after inhalation of particles < 5 micrometer of spores) usually manifest with the following symptoms/Signs: fever, diaphoresis, headache, fatigue and malaise, nonproductive cough, mild chest discomfort, severe respiratory distress with dyspnea, stridor, cyanosis, and shock. Without treatment, death typically occurs within 24-36 hours after onset of severe symptoms. The diagnosis is made with the assistance of chest X-rays showing a widened mediastinum. A Gram stain of the blood and blood culture is also used to identified the bacillus.
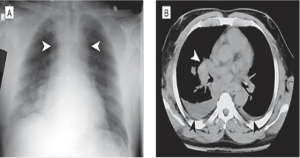 |
|
| “Image of a Patient with pulmonary Anthrax” – Widened mediastinum (white arrowheads) – Hilar lymph node (white arrowhead in CT image). |
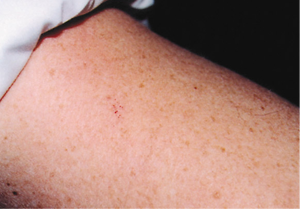
Cutaneous Anthrax
 |
| “Image of cutaneous anthrax,” from JAMA article,[29] Fair Use. |
Since the major affected area is the skin, there is no constitutional symptoms, local itching with an hemorrhagic gelatinous papulae, raised, depressed thick necrotic scar with surrounding brawny edema – painless – Heals with little scarring. If disseminated, edema of the head and neck interfering with breathing, vision and swallowing.
When referring to the treatment for anthrax and other biological agents , antibiotics are usually the treatment of choice. Most of the bacterial agents respond successfully to Ciprofloxacin or Doxycycline. Antibiotics used for treatment are also used for prophylaxis (to avoid the risk of secondary transmission, especially for health care workers). Vaccines are available for some of the agents (For all agents, see handout’s table of treatment for biological agents)
Smallpox
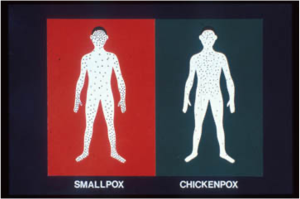 |
| Smallpox or Chicken Pox? Body localization shows the difference. Minnesota Department of Health,[30] Public Domain. Also, From http://www.who.int/emc/diseases/smallpox/slideset/index.htm
|
Smallpox is a highly contagious disease caused by the Orthopox virus. The potential threat as a WMD is attributed to the aerosol infectivity of the virus. The incubation period for smallpox is 7 – 19 days (Average 10-12). The disease has a duration of 4 weeks. The Case Fatality Rate (CFR) of smallpox is 1 – 30 %. If there is an hemorrhagic form the CFR is 96-100%. The signs/Symptoms of smallpox include malaise, fever, vomiting, headache, and backache. The characteristic skin lesions are the papules that appear after the 2- 3 days of fever, these papulaes progress to pustular vesicles that are abundant on face and extremities, and develop synchronously. If the person has been previously vaccinated, few atypical lesions appear and the disease follows an accelerated course. The Diagnosis requires clinical exam and laboratory (a PCR that identifies the orthopoxivirus).
Smallpox has a characteristic temperature cycle, which can be better understood by looking to a typical temperature chart. (See image). The evolution of smallpox is also characteristic (See pictures of a child with smallpox).
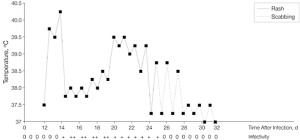 |
Image of Smallpox in a child – source of the picture below.
|
| Temperature chart of a patient with Smallpox Day 14 Temperatures of 40.5 C (104.9 F) Or 39.5 C (103.1 F) by Day 12
Infection, it shows the approximate time of appearance, evolution of the rash, and magnitude of infectivity relative to the number of days after the patient acquire the infection. (From JAMA 9, 1999 –Vol 281, No. 22, 2127). Both images are from JAMA article,[31], Fair Use. Henderson DA, Inglesby TV, Bartlett JG, et al. Smallpox as a Biological Weapon: Medical and Public Health Management. JAMA. 1999;281(22):2127–2137. doi:10.1001/jama.281.22.2127 Smallpox in a child. The pictures show (from left to right), days 3, 5, and 7 of evolution of a typical case of Smallpox in a child. (From Henderson et al. JAMA, June 9, 1999 – Vol 281, No 22, 2127. |
|
Smallpox Vaccination – A 3 Steps Process
 |
 |
 |
| Step 1: Vaccination is done with the bifurcated needle. The requisite amount of reconstituted vaccine is held between the prongs of the needle. | Step 2: The vaccination process continues by doing multiple punctures (15 strokes), at right angles to the skin over the deltoid muscle. | Step 3: The multiple punctures are rapidly made within an area of about 5 in diameter.
(Pictures taken from Henderson et al. JAMA, June 9, 1999 – Vol 281, No 22, 2127).[32] |
Plague
 |
| Yersenia pestis is a Gram – bacilli identified by Wright-Giemsa stain, showing its characteristic bi-polar staining“Yersinia pestis,” image from CDC, Public Domain.Note: image from Wayson stain showing the characteristic “safety pin” appearance of Yersinia pestis, the plague bacillus. Image courtesy of Centers for Disease Control and Prevention (CDC), Atlanta, Ga. |
The agent for plague is the Yersinia pestis bacterium, and it is usually identified by laboratory tests such as a Gram/Giemsa of sputum, and culture. Plague is a disease of rodents accidentally transmitted to humans by the bite of an infected rat flea. The disease can be presented in two forms: pneumonic (pulmonary) and bubonic (lymph nodes). What make plague a potential WMD? The answer is, the purposeful aerosol dissemination of the plague agent. If untreated, plague has a high mortality, killing the affected individual in a period of 12-24 hours. The signs/symptoms start after an Incubation period of 1-6 days, these symptoms include high fever/chills, headache and malaise, frequently accompanied of cough/hemoptysis (blood), dysnea, stridor, cyanosis, respiratory failure.
Clinical Manifestations of Plague
 |
 |
| “Common lesions in plague. Patient with bubo (enlarged, inflamed lymph node) on the neck,” image from JLGH, same reference as the contigous picture about gangrene associated with plague. | “Gangrene-induced necrosis on the toes of a patient with plague,” image from an article from JLGH,[33], Fair Use.
This new updated images come from Eastman, TE. (2009). The Making of a Pandemic: Bubonic Plague in the 14th Century. JLJC –Journal of Lancaster General Hospital. From https://www.jlgh.org/Past-Issues/Volume-4-Issue-1/The-Making-of-a-Pandemic.aspx |
Tularemia
The agent for Tularemia is known as Francisella tularensis. Tularemia is transmitted by ticks/deer flies or direct contact with infected rodents. The disease Incubation Period is 1- 10 days with a duration of the disease approximated of 2 weeks. If untreated Tularemia has a 10- 35% mortality. The disease has mainly two forms: ulceroglandular and typhoidal (systemic). Common signs/symptoms of ulceroglandular tularemia include local ulcer and regional lymphadenopathy accompanied of fever, chills, and malaise. Besides the typical signs and symptoms, the diagnostic is made using the following Laboratory tests: serology; blood cultures; PCR; IGG & IGM, Agglutination Reaction. Chest X-rays.
 |
 |
| “Francisella tularensis,” image from CDC, Public Domain.
a gram negative coccobacillus poorly stained-by nature |
“Lymphadenitis,” image from Vinmec, Fair Use.
Ulceroglandular Tularemia: this patient has lymphadenitis and pharyngeal Tularemia |
Typhoidal Tularemia, this form of the disease has the characteristic signs/symptoms, fever, headache, and malaise. Usually in this type of tularemia, there is no visible adenopathy, sub-sternal discomfort, non-productive cough, andprostration. In Typhoidal Tularemia, the affected person develops pneumonia (multiple infiltrates) with pleural effusion.
 |
| “Chest-x-rays of pneumonia caused by typhoidal tularemia,” image from CDC, Public Domain. |
The treatment of tularemia is antibiotics such as Streptomycin or Gentamycin. Post-Exposure Prophylaxis: Doxycycline/Ciprofloxacin. There is no vaccine for tularemia but there is an investigational vaccine has been given to > 5,000 persons without significant adverse reactions. It prevents typhoidal and ameliorates ulceroglandular forms of laboratory-acquired tularemia.
Botulinum and Botulism
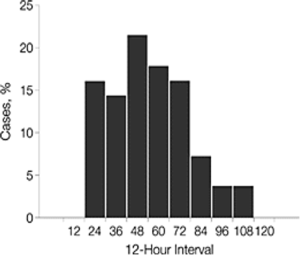 |
| Graph of an Outbreak of Botulim in Michigan 1977- 59 persons presented Botulism after eating at a restaurant with contaminated food
“Graph of an Oubreak of Botulinum in Michigan, US 1977,” Image from JAMA article,[34] Fair Use. |
In general, an outbreak of botulism has a characteristic presentation that can be clinically and epidemiological observed (see picture of the characteristic graph of the frequency of cases); the onset of symptoms start approximately after 12-18 hours of exposure and continued with a maximum peak after 48 hrs of exposure to the toxin.
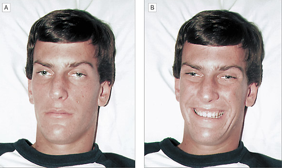 |
| “Image of a young individual with botulinum affected face muscles,” image from JAMA article,[35], Fair Use.
Observe the 'mask' expression due to the contraction of the face muscles. |
Clinical manifestations include the following signs/symptoms of Botulism, ptosis, blurred vision, diploplia (double vision), dry mouth and throat, dysphagia, and dysphonia. It is characeteritic to find symmetrical descending flaccid paralysis, and in some cases, the disease can progress to respiratory failure, reason for what botulism is considered a medical emergency. Additional clinical characteristics of botulism is that there is no fever, the person tends to remain alert, postural hypotension is commonly found, and for the eyes, pupils appear unreactive. Sensation is normal sensation although variable muscle weakness is presented. The laboratory tests used for diagnosis include serology (blood tests), toxin assays, anaerobic cultures: blood/stool; and electromyography. Prophylaxis: a pentavalent toxoid vaccine is available for those at high risk of exposure.
Filoviruses (Marburg, Ebola)
 |
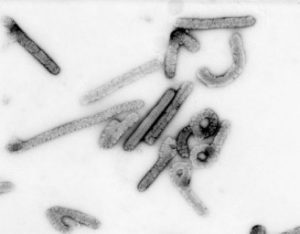 |
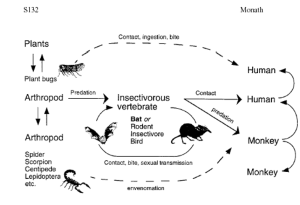
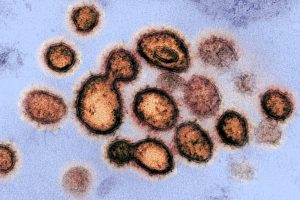
| "Monkey is a reservoir," Image from a Presentation on Malaria in Africa, Public Domain. | "Ebola (Marburg) virus," electronic picture from Wikimedia Commons, Public Domain. |
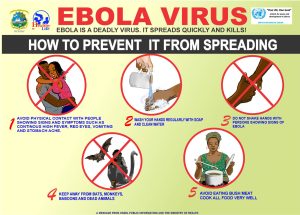
These viruses have an unknown natural reservoir, primates become the accidental host; and the infection is spread by person to person contact. The mode of transmission is by contact with body fluids (e.g., blood, saliva, and urine) of an infected person or animal. The disease has an Incubation Period of 2 - 19 days (average 4-10 days), and the duration of disease varies from days to weeks. The Case Fatality Rate is > 80%. The disease has never been seen in the US.
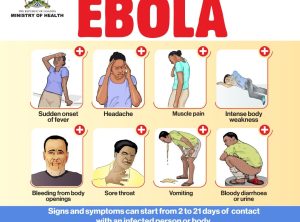 |
| "Ebola - symptoms," image from a prevention campaign in Uganda, Africa, Public Domain. |
Outbreaks
The map below and also the diagram reports historical information of major outbreaks, the most recent outbreak of Ebola in Liberia is not included in these images, but it will included later in the content of this chapter.
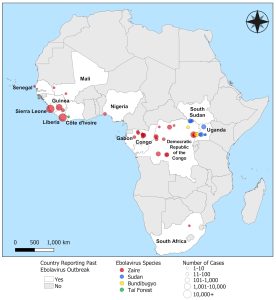 |
| "Ebola Disease Outbreaks by Species and Size, Since 1976" [36] image from CDC, Public Domain. |
Marburg Virus Outbreaks
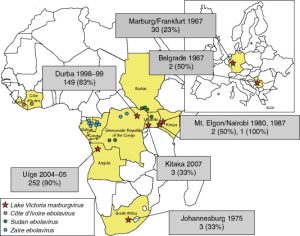 |
| "Marburg virus oubreaks," image of African points with reported outbreaks from Science Direct,[37] Fair Use.
Note: Location of known filovirus outbreaks. Countries that have experienced occurrences of filoviruses are indicated in yellow. For MARVs, the location of the outbreak is indicated by a red star. The main center (city/village) of the outbreak is indicated, along with the year of the outbreak, the number of cases, and the case–fatality rate (indicated in brackets). Incidents of the various EBOV species are also indicated. |
 |
| "Nurse and Ebola patient", image from Wired, Fair Use. |
During October 1, 2004--March 29, 2005, a total of 124 cases were identified; of these, 117 were fatal, and approximately 75% of the reported cases occurred in children aged <5 years. Cases also have occurred in adults, including health-care workers. Predominant symptoms have included fever, hemorrhage, vomiting, cough, diarrhea, and jaundice.[38]
Marburg virus - presentation of the disease
 |
|
"Maculopapular rash in Marburg disease," image from Borio et al., 2002, JAMA.[39],Fair Use. |
Marburg virus disease presents as an acute febrile illness and can progress within 6--8 days to severe hemorrhagic manifestations. After an incubation period of 5--10 days, onset of the disease is sudden and is marked by fever, chills, headache, and myalgia. Approximately the 5th day after onset of symptoms, a maculopapular rash might occur, after which nausea, vomiting, chest pain, sore throat, abdominal pain, and diarrhea might appear. Signs and symptoms become increasingly severe and can include jaundice, inflammation of the pancreas, severe weight loss, delirium, shock, liver failure, massive hemorrhaging, and multi-organ dysfunction.
Prevention measures for Marbug virus
Recall: this section of the chapter is about the use of Radiological, Chemical or Biological agents that can be potentially used as Weapons of Mass Destruction (WMD). The following content focus on the use chemical agents as WMD.
Terrorist Attacks using Chemicals agents
 |
| "A worker in a protective suit inspects 122mm sarin rockets at an undisclosed location in Iraq in this Oct. 1991," handout picture from the United Nations. (AP / UNSCOM), Fair Use. |
There is at least fifty-two (52) chemical agents that can be potentially used as Weapons of Mass Destruction (WMDs). Among all these chemical agents, there is a group of agents known as as nerve agents, which include, sarin, ricin and mustard gas. They represent the most common chemical agents that have been reported to be used as WMDs, and that still have the potential to be used for chemical terrorist attacks in the future. Nerve agents are the most toxic and rapidly acting of the known chemical warfare agents. They are similar (because of their acting mechanism and body’s damage) to organophosphates pesticides. However, they are much more potent than organophosphate pesticides. As a historical fact, sarin and other nerve agents may have been used in chemical warfare during the Iran-Iraq War in the 1980s
Sarin
|
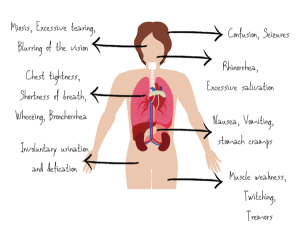
| "Symptoms of nerve agents," image from EMResident, Fair Use. |
Sarin and other nerve agents may have been used in chemical warfare during the Iran-Iraq War in the 1980s. Sarin was originally developed in Germany (1938) as a pesticide. It is a water soluble liquid and the most volatile of the nerve agents. Exposure to Sarin can happen through: skin or eye contact, by breathing air that contains sarin, touching or drinking contaminated water with sarin, and several other routes such as by eating Sarin-contaminated food, through clothes of a person exposed to Sarin’s vapors (it last for about 30 minutes). Depending of the situation, exposure to vapors: symptoms appear within a few seconds. While exposure to liquid form (it takes up to 18 hours to develop symptoms). In general it is accepted that people exposed to mild/moderately exposure will recover completely, but if there are individuals who become severely exposed, they will be not likely to survive.
What are the major signs/symptoms of Sarin’s exposure?
Common symptoms of sarin's exposure are mainly manifested on the eyes and the respiratory system, when it is affecting the eyes, the persons shows pinpoint pupils, watery/painful eyes, miosis ( blurred vision). Nasal symptoms are also common, these may include, an increased on secresions also known as rhinorrea. Respiratory/cardiac symptoms include: shortness of breath, coughing, chest tightness, tachipnea, tachicardia, low/high blood pressure. Additional manifestations of exposure to sarin include, excessive sweating, excesive urination, nausea, vomiting, abdominal pain alone or with diarrhea. Also, central nervous system symptoms such as confusion, drowsiness, weakness, headache, etc.
What to do in case of exposure to Sarin
People exposed to sarin should be taking at the closest medical center emergency department, but in the meantime some general measures can be taken, these are, removing the victim's clothes, clothes that has to be pulled over the head should be cut off, deposit contaminated clothes in a plastic bag/Do not handle them, and probably at the hospital level the rest of the following recommendations need to be done: washing any liquid Sarin from the skin with large amounts of soap and water. If eyes are burning or if vision is blurred, rinse them with plain water for 10 to 15 minutes, and if Sarin has been swallowed, it is recommended to not induce vomiting or give fluids to drink.
Ricin
 |
 |
| "The castor plant (Ricinus communis)", image from Wikimedia Commons, CC BY-SA 4.0 -it is from this plant that the oil is extracted. | "Ricin oil", image from Wikimedia Commons, CC BY-SA 4.0 |
As mentioned before, ricin is another common nerve agent that has the potential to be used for terrorist attacks. Ricin is a potent toxin made from the castor plant and is usually available as 'ricin oil'. Exposure to Ricin can occuring from several routes of exposure, for example, dermal/mucoses/inhalation (mist or powder), ingestion (contaminated water), or injection (pellets/liquid - 500 mcgr. enough to kill adult). The symptoms of exposure for example through skin (dermal) or mucoses are redness and pain of the skin/eyes. When inhaled - in 4-8 h- acute onset of fever, respiratory symptoms: chest tightness, cough, dyspnea. If the person does not receive treatment after 36-72 hours of exposure, hypoxia and respiratory failure can occur. When ricin is ingested- nausea, vomiting, bloody diarrhea, severe dehydration and low blood pressure can be the main manifestations. In addition, CNS symptoms such as hallucinations or seizures can occur. In serious cases after exposure to ricin, blood in the urine and complete vascular collapse and death occurs too. There is no effective prophylaxis for exposure to ricin, and this because there is currently no vaccine or prophylactic antitoxin available for human use.
What to do in case of exposure to Ricin
The general measure if to wear a protective mask to prevent inhalation. Ricin is nonvolatile, and secondary aerosols are not expected to be danger to first responders or any other type of health care providers. Once the contaminated person arrives to the emergency room, the first step is to decontaminate the exposed person with soap and water. It is known that hypochlorite solutions (0.1 % sodium hypochlorite) inactive ricin. Having this type of solution is beneficial to health care worker in the case of an event exposure to ricin.
Blister agents: Mustard Gas
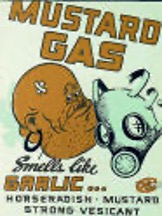 |
| "Mustard Gas", Poster using during WWII,image from Wikimedia Commons, Public Domain. |
Blister agents such as mustard gas are vesicant substances with slight garlic/mustard odor. It is known that sulfur mustards vapors are heavier than air evaporating slowly, water and oil soluble. Knowing these characteristics is always important to recognize and the agent and its possible effects if an exposure occur. For example, the major route of exposure to mustard gas is, vapor’s inhalation (respiratory tract) which is the faster route of exposure. Other routes of exposure such the skin/eye and mucous membranes takes more time to develop symptoms. Ingestion (if liquid) is also relatively slower compared to inhalation. It is important to note that the clinical effects of exposure to mustard gas do not occur until hours after exposure. The median incapacitating dose for the vapor is 200 mg-min/m. A Ct of 12 to 70 mg-min/m produces eye lesions, and direct contact with the liquid can cause skin and eye burns that develop an hour or more after exposure. A 10 µg droplet is capable of producing blisters.
What are the major Signs and Symptoms of exposure to Mustard Gas
 "Soldier exposed to mustard gas during WWI -1917", image from Governmental website The Capture of Vaux, Public Domain. |
Symptoms after exposure to mustard gas may not occur for 2 to 24 hours. Usually exposure is not fatal, when symptoms occur the most common affect the skin, eyes, respiratory and digestive tract. In the case of skin exposure: redness/itching and eventually yellow blistering occur as one of the most frequent manifestation. When the eyes are affected, it happens usually between 3-12 hours and these include - irritation, pain, swelling, and tearing. Severe exposure may cause symptoms 1-2 hours producing light sensitivity, severe pain, or blindness (lasting up to 10 days.). In addition, respiratory symptoms can be rhinorrea (running nose), sneezing, bloody nose, sinus pain, shortness of breath, and cough. If the exposure affects the digestive tract, it is commonly manifested by abdominal pain, diarrhea, fever, nausea, and vomiting. When extensive skin burning occurs, it can be fatal that is one of the main reasons to wear protective clothes and take the necessary measures before receiving medical care. Getting fresh air, evacuation of buildings, changing clothes and body washing are in general important measures to avoid more serious consequences of the exposure to mustard gas.
On the other hand, there are long-term health effects of exposure to mustard gas and these include, scarring as a consequence of the second- and third- degree burns occurred from the exposure. Other long term effect is chronic respiratory disease that comes from extensive breathing in of the mustard gas vapors; blindness due to extensive eye exposure
Things to consider in the case of possible exposure to a chemical agent
- If a person reports exposure to a possible agent: Ask yourself: what is the possible chemical agent?
- EMS personnel reports the presence of a liquid on victim's skin/clothes or any special odor.
- What are the symptoms developed by the patient during transportation to the Emergency Room?
- Do signs and symptoms correspond with chemical agents? Check available protocols and other sources of information.
Radiological and Nuclear Agents
A brief review of important concepts. Before more information is provided for this section, the question is, what is radiation? The term radiation refers to “Energy traveling through space. Some types of radiation associated with radioactivity are alpha and beta particles and gamma and X rays.” There are two types of radiation, ionizing and non-ionizing. Non-Ionizing is longer wavelength/lower frequency energy. And, Ionizing radiation is short wavelength/high frequency higher energy.
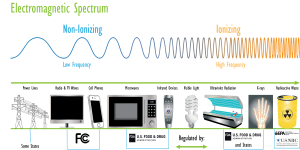 |
| "Electromagnetic Spectrum," image from EPA, Public Domain.
|
Another concept that is useful to review is the level of penetration of ionizing radiation in human flesh. See image below.
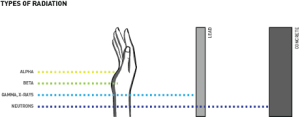 |
| "Types of Radiation", image from Sutori, Fair Use. Penetration level of radiation in human flesh, a comparison with some flesh, lead and concrete barriers. |
There is a potential use of the following for terrorist attack using radiological agents.
 |
| "Radiological Dispersal Device", image from Etox University of Idaho, Fair Use. |
A Dirty Bomb. The threat for radiological agents could be a “dirty bomb” - a dispersion device (RDD) that combines dynamite + radioactive materials (powder or pellets) obtained from hospitals, construction sites or food irradiation plants. The idea behind a dirty bomb is to blast radioactive material into the area around the explosion causing buildings and people to be exposed to radiation because the source of the radiation is unknown, it is difficult to measure how much radiation might be present. However, at the levels created by most probable sources, not enough radiation would be present in a dirty bomb to cause severe illness from the exposure.
What to do - and explanations
Particle Dispersion
 |
| "Dispersion area," image from source not available English speaking source. It is from the document censored in the Internet. Image included just for explanation of the concept of particle dispersion. |
Radioactive particles from nuclear devices and “dirty bombs” can spread across a .wide geographic area.
Signs and Symptoms of radiation’s exposure
Additional clinical features
Lymphocyte counts decrease within the first week after an acute whole body exposure, depending on the absorbed dose to the body and the consequent severity of (acute) radiation sickness. Laboratory: lymphopenia within 8-24. Treatment is supportive with fluids, antibiotics, and transfusions stimulating factors. If there are early CNS findings or unexplained hypotension, survival is unlikely.
If people are not too severely injured by the initial blast. People need not to leave the immediate area on foot
Additional sources of Emergencies: Epidemics and Pandemics.
The history of epidemiology and public health has been shaped by the presence of pandemics: plague, flu, and recently, coronavirus or, COVID-19. Throughout history, these pandemics have been responsible for the death of thousands of people around the world. Overall, what has changed from ancient times to today's public health is the availability of vaccines, and the improvement in water and sanitation around the world, with major gains for developed nations who have better systems of drinking water, and sanitation. Until recently, the fear of a major pandemic has been for a worldwide-scale flu that could kill thousands of people. But instead of the flu, the world received the coronavirus pandemic, which is still around. Since flu has been the major fear before the coronavirus, this section will cover some of the major events of flu pandemics.
Flu pandemics
In general, flu pandemics have been repeated in history every 100 years, and because of that the 'expected' and 'predicted' pandemic was on flu (and not coronavirus).[41]. Because of its importance in history, the first major pandemic that appears usually in most history books is the flu pandemic.
The flu pandemic of 1918
The 1918 Influenza (flu) Pandemic (also called, the Spanish flu, because of the great mortality in that country at that time). This famous pandemic lasted from 1918-1919 and killed 50 to 100 million persons worldwide. The pandemic had three waves as it is represented in the following image:
 |
|
"1918 spanish flu waves," Image Licensed Public Domain, Wikipedia. |
The 2009 H1N1 influenza pandemic: a repeat of the 1919 pandemic
The specific time of this pandemic is from 2009-2010. The disease was first identified in the United States and eventually was named the 2009 H1N1 influenza. The first two cases of the disease were reported by the Centers for Disease Control and Prevention (CDC) in April 2009, after this, the number of cases grew to 60 million by summer 2010. The pandemic also attacked several other countries in the world, and it was known to prefer the group of people 14-64 years, with those aged 65 and older as the less affected group.[44], [45] This pandemic should have served as a lesson for the U.S., but a lot of skepticism grew that the possible for another major pandemic was not possible, or, if this would happen then, the country had enough public health resources including vaccines to control the problem, which has been proven wrong with the current coronavirus pandemic making manifest that the U.S. public health system was not prepared for a pandemic.
 |
The prediction of a new pandemic was always there but the medical and public health preparations were never in place, so, the pandemic started in Wuhan, China with several infected persons never seen before, the agent coronavirus named COVID-19 because of the year in which it was reported as the cause of the pandemic. The news was everywhere, but the United States did not pay attention to the situation, until almost two months later in March 2020; acknowledging and responding to the pandemic was proven bad, because the country and the world did not have a vaccine for it, nor the U.S. had the public health infrastructure to respond properly, there was a lot of unknown about the disease, and especially its form of transmission; the measures taken since the beginning did not have a social acceptance in a society that values so much its personal freedom, and having the federal government, and public health authorities, and experts tell the public to wear a mask, stay at home and related mandates created an epidemic of misinformation, and contradictory messages that have been hard to eliminate until today.[48],[49]. I have found an image -shown below that summarizes some of the reasons for this campaign of misinformation that has been one of the major problems of the COVID-19 pandemic.
 |
| "Fast-Slow-Science," By Dasaptaerwin, Licensed CC 4.0 International, Wikimedia Commons. There is also an article that refers to more details about the content of the image.[50] |
 |
| "Global distribution of estimated excess mortality rate due to the COVID-19 pandemic, for the cumulative period 2020–21" Image from an article by Haidong Wang, H., Paulson, KR., Pease, SA., Watson, S. et al.[54] |
Prevention and Control of Emergencies during Epidemics and Pandemics
The essential methods used commonly to prevent an infectious disease are also used during epidemics and pandemics, these methods include the use of vaccines, sanitation, isolation, quarantine, and additional measures that have been used for centuries but are becoming relevant with the COVID-19 worldwide pandemic.
In addition, there are three key factors that are considered essential, 1) Remove, eliminate, or contain the cause or source of infection, 2) Disrupt and block the chain of disease transmission, and 3) Protect the susceptible population against infection and disease. In this context, an additional set of recommendations is also prescribed, and discussed in the following paragraphs:
Vaccines (also, called, Immunizations)
In the history of medicine and public health (including, epidemiology), vaccines have been considered the major weapons of defense, especially in the prevention of infectious diseases, especially those common childhood infectious diseases. [55] See below a list of common vaccines that are available:
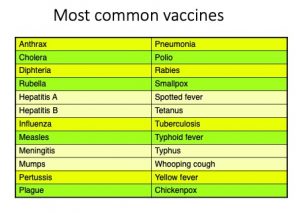 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
 |
| "How vaccines work," image from World Health Organization (WHO), Licensed Public Domain. |
Sanitation
Hand washing has been the oldest of the measures used to prevent infection. For centuries, public health has promoted hand washing as the number one activity to keep people out of disease (infectious disease).[58], [59]Together with this measure, it is important to pay attention to personal hygiene (frequent bathing, regular
 |
| 'Hand washing' image from Pixbay. |
grooming, teeth cleaning, and maintenance, changing clothes frequently), and to keep ventilation in homes, and buildings as the cleaning of surfaces that can act as Fomite(s) or, inanimate transmitters of an infectious agent.[60]
In addition, face mask covering and personal protective equipment or PPE are also considered
 |
| Family mask, image from Pixabay. |
especially for healthcare workers who are considered more at risk due to their exposure with infected clients, and surfaces.[61]
Environmental controls to prevent infectious diseases
This measure is aimed at providing clean and safe air, water, milk, and food. It also includes the management of solid waste (trash, and garbage); liquid waste (sewage); and control of vectors (insects and rodents) of disease.
Host-related control & prevention
Based on the concept model of the epidemiological triangle of infection, the host-related control is intended to protect the host from contagious diseases and infections the following protective measures are used: quarantine and isolation.
Quarantine
The original meaning of this word is that quarantine means, forty days, however in recent years, the word quarantine refers to specific amount of time considered in which a person is isolated, or, separated from those who are not infected with the agent, and it is not necessarily forty days, it can be as short a week, two weeks, depending on the situation as it has been used during the COVID-19 pandemic. [62], [63]
 |
| 'Quarantine', image from PNGmart. |
In addition, it accepted that there are four levels of quarantine used in public health: 1) Segregation, 2) Personal surveillance, 3) Modified quarantine, 4) Complete quarantine. Most of the mentioned levels are very much self explanatory but more details can be found in the Internet and epidemiology and public health literature. [64]
Isolation
This method is mainly used for limited number of cases as it is in the case of humans, and also for animals. There are six levels of isolation: 1) In a private isolation room, 2) The use of separate and infection control gowns, 3) Staff must wear masks, 4) All staff must gloved with interacting, treating, or working
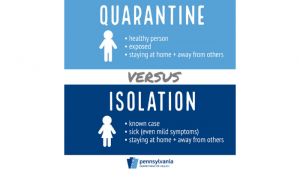 |
| ‘Quarantine versus isolation’, Image from Dept. of Health, City of Philadelphia, Pennsylvania. |
with or on the patient or subject (e.g. an animal), 5) Hands washing is required upon entering, and leaving the patient’s room, 6) All contaminated articles or possible contaminated articles including linen, dressing, syringes, instruments, etc., must be disposed properly.[65]
Summary
This chapter has covered the most essential concepts and definitions about emergency response and disaster preparedness with an extensive emphasis on the use of the Incident Command System (ICS) as an important tool used mainly by first responders to organize effective communication and organizational response to an emergency. The training of public health workers in the area of emergencies have been also covered, putting emphasis in the role of public health workers during emergencies and disasters. The last two sections of the chapter have focused on Weapons of Mass Destruction such as biological, chemical, radiological/nuclear that can create emergencies due to potentially terrorist attacks in the nation. This topic is followed by a general view of the role of public health during pandemics and the implementation of prevention and control such as vaccinations, sanitation and quarantine.
- Wikipedia. (n.d.). Emergency. From https://en.wikipedia.org/wiki/Emergency ↵
- Wikipedia. (n.d.). Preparedness. From https://en.wikipedia.org/wiki/Preparedness ↵
- Ready. (n.d.). Disasters and Emergencies. From ↵
- Cornell Law School. (n.d.). Emergency. From https://www.law.cornell.edu/wex/emergency ↵
- International Federation of Red Cross and Red Crescent Societies (IFRC). What is a Disaster? From https://www.ifrc.org/our-work/disasters-climate-and-crises/what-disaster ↵
- de Anda HH, Freeman CL, Braithwaite S. (2024). EMS Criteria for Disaster Declaration. In: StatPearls [Internet]. From: https://www.ncbi.nlm.nih.gov/books/NBK539803/ ↵
- The National Society of Leadership and Success (NSL).(n.d.). Learn, Lead, Succeed. From https://www.nsls.org/ ↵
- Federal Emergency Management Agency (FEMA). (2019). Acronyms and Abbreviations. From https://www.fema.gov/about/glossary ↵
- American Medical Association and the National Disaster Life Support Foundation. (n.d.). The DISASTER Paradigm, Lesson Six. From https://yanktonruralahec.org/wp-content/uploads/2015/11/CDLS-2015-Lesson-6-The-DISASTER-Paradigm.pdf ↵
- Definition of ICS taken from New York State Department of Health. (n.d.). Introduction to the Incident Command System. From https://www.health.ny.gov/professionals/ems/pdf/srgics.pdf ↵
- U.S. Department of Transportation Federal Highway Administration Office of Operations. (2023). Simplified Guide to the Incident Command System for Transportation Professionals. From https://ops.fhwa.dot.gov/publications/ics_guide/ ↵
- New York State Department of Health. (n.d.). Introduction to the Incident Command System. From https://www.health.ny.gov/professionals/ems/pdf/srgics.pdf ↵
- Federal Emergency Management Agency (FEMA). (n.d.). Module 3: unit iv — planning functional training. From https://www.fema.gov/pdf/emergency/usr/mod3_u4.pdf ↵
- Mississippi Emergency Management Agency. (n.d.). Overview of the Logistics Section and the Facilities Unit, Unit 2 Student Guide. From https://www.msema.org/wp-content/uploads/2018/10/05_FACL_Unit02_SG.pdf ↵
- Content from this section has been prepared using another reference listed above: American Medical Association and the National Disaster Life Support Foundation. (n.d.). The DISASTER Paradigm, Lesson Six. From https://yanktonruralahec.org/wp-content/uploads/2015/11/CDLS-2015-Lesson-6-The-DISASTER-Paradigm.pdf ↵
- Federal Emergency Management Agency (FEMA). (n.d.). Incident Command System (ICS), Lesson 4, Overview. From https://emilms.fema.gov/is_0200c/groups/450.html ↵
- Federal Emergency Management Agency (FEMA). (n.d.). Incident Command System (ICS), Lesson 2, Overview. From https://emilms.fema.gov/is_0200c/groups/447.html ↵
- USDA. (n.d.). ICS 300 Lesson 4: Unified Command. From https://www.usda.gov/sites/default/files/documents/ICS300Lesson04.pdf ↵
- First Responders First. (2021, March 24). Who is a First Responder? From https://www.firstrespondersfirst.com/post/what-is-a-first-responder ↵
- ID.me Help Center. (n.d.). First responder eligibility. From https://help.id.me/hc/en-us/articles/202293510-First-responder-eligibility ↵
- Office of Homeland Security. (n.d.). National Terrorism Advisory System. From https://www.dhs.gov/national-terrorism-advisory-system. ↵
- Public Health Foundation (PHF). (n.d.). Public Health Preparedness and Response, Public Health Preparedness and Response Core Competencies. From https://www.phf.org/programs/preparednessresponse/Pages/Public_Health_Preparedness_and_Response_Core_Competencies.aspx ↵
- United States Department of Justice Archives. (n.d.). Ten Years Later: The Justice System after 9/11. From https://www.justice.gov/archive/911/ ↵
- Congressional Research Service. (May 22, 2019). Federal Grants to State and Local Governments: A Historical Perspective on Contemporary Issues. From https://sgp.fas.org/crs/misc/R40638.pdf ↵
- CDC. (2018). Public Health Emergency Preparedness and Response Capabilities: National Standards for State, Local, Tribal, and Territorial Public Health. From https://www.cdc.gov/orr/readiness/capabilities/index.htm ↵
- CDC. (2020). Anthrax as a Bioterrorism Weapon [the definition of bioterrorism is included at the top of the content of this article]. From https://www.cdc.gov/anthrax/bioterrorism/index.html ↵
- Image for the bacillus antracis. Article by Inglesby, T., O'Toole, T., Henderson, D., Bartlett, J., et. al (2002). Anthrax as a Biological Weapon, 2002. Updated Recommendations for Management, JAMA, 287 (17), 2236. 10.1001/jama.287.17.2236. From https://pubmed.ncbi.nlm.nih.gov/11980524/ ↵
- Borio, L.L., Frank, D., Mani, V., Chiriboga, C., Pollanen, M., Ripple, M.G., Ali, S., DiAngelo, C.R., Lee, J., Arden, J., Titus, J.L., Fowler, D., O'Toole, T., Masur, H., Bartlett, J., & Inglesby, T.V. (2001). Death due to bioterrorism-related inhalational anthrax: report of 2 patients. JAMA, 286 20, 2554-9 . ↵
- Freedman A, Afonja O, Chang MW, et al. Cutaneous Anthrax Associated With Microangiopathic Hemolytic Anemia and Coagulopathy in a 7-Month-Old Infant. JAMA. 2002;287(7):869–874. doi:10.1001/jama.287.7.869. From https://jamanetwork.com/journals/jama/article-abstract/194656 ↵
- Minnesota Department of Health. (n.d.). Characteristic Rash of Smallpox. PowerPoint Presentation, slide 20. From https://www.health.state.mn.us/diseases/smallpox/spslides.pdf ↵
- Henderson DA, Inglesby TV, Bartlett JG, et al. Smallpox as a Biological Weapon: Medical and Public Health Management. JAMA. 1999;281(22):2127–2137. doi:10.1001/jama.281.22.2127 ↵
- Henderson DA, Inglesby TV, Bartlett JG, et al. Smallpox as a Biological Weapon: Medical and Public Health Management. JAMA. 1999;281(22):2127–2137. doi:10.1001/jama.281.22.2127 ↵
- Eastman, TE. (2009). The Making of a Pandemic: Bubonic Plague in the 14th Century. JLJC –Journal of Lancaster General Hospital. From https://www.jlgh.org/Past-Issues/Volume-4-Issue-1/The-Making-of-a-Pandemic.aspx ↵
- Arnon, S.S., Schechter, R., Inglesby, T.V., Henderson, D.A., Bartlett, J.G., Ascher, M.S., Eitzen, E.M., Fine, A.D., Hauer, J.M., Layton, M., Lillibridge, S.R., Osterholm, M.T., O'Toole, T., Parker, G.W., Perl, T.M., Russell, P.K., Swerdlow, D.L., & Tonat, K. (2001). Botulinum toxin as a biological weapon: medical and public health management. JAMA, 285 8, 1059-70 ↵
- article,[footnote]Arnon, S.S., Schechter, R., Inglesby, T.V., Henderson, D.A., Bartlett, J.G., Ascher, M.S., Eitzen, E.M., Fine, A.D., Hauer, J.M., Layton, M., Lillibridge, S.R., Osterholm, M.T., O'Toole, T., Parker, G.W., Perl, T.M., Russell, P.K., Swerdlow, D.L., & Tonat, K. (2001). Botulinum toxin as a biological weapon: medical and public health management. JAMA, 285 8, 1059-70 ↵
- CDC. (2023). Ebola Disease Distribution Map: Cases of Ebola Disease in Africa Since 1976. From https://www.cdc.gov/vhf/ebola/history/distribution-map.html ↵
- Falzarano, D., Feldmann, H. (2008). “Marburg Virus,” in Encyclopedia of Virology (Third Edition). Chapters and Articles. From https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/marburgvirus ↵
- CDC, MMR Reports. (2005, March 29). Brief Report: Outbreak of Marburg Virus Hemorrhagic Fever --- Angola, October 1, 2004--March 29, 2005. MMR 54(Dispatch);1-2.From https://www.cdc.gov/mmwr/preview/mmwrhtml/mm54d330a1.htm ↵
- Borio et al. (2002). Hemorrhagic Fever Viruses as Biological Weapons: Medical and Public Health Management. JAMA 287 (18), 2391. DOI: 10.1001/jama.287.18.2391 ↵
- Ligon B. L. (2005). Outbreak of Marburg hemorrhagic fever in Angola: a review of the history of the disease and its biological aspects. Seminars in pediatric infectious diseases, 16(3), 219–224. https://doi.org/10.1053/j.spid.2005.05.001 ↵
- Kertscher, T. (April 10, 2020). Fact-check: Has a pandemic occurred every 100 years? PolitiFact. From https://www.statesman.com/story/news/politics/elections/2020/04/10/fact-check-has-pandemic-occurred-every-100-years/984128007/ ↵
- Taubenberger, J. K., & Morens, D. M. (2006). 1918 Influenza: the mother of all pandemics. Emerging infectious diseases, 12(1), 15–22. https://doi.org/10.3201/eid1201.050979 ↵
- Barry, J. M. (2020). The great influenza: The story of the deadliest pandemic in history. Penguin UK. ↵
- CDC. (no date). 2009 H1N1 Pandemic (H1N1pdm09 virus). From https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html ↵
- Mayo Clinic Staff. (Feb 24, 2021). H1N1 flu (swine flu). From https://www.mayoclinic.org/diseases-conditions/swine-flu/symptoms-causes/syc-20378103 ↵
- Branswell, H. (June 11, 2019). The last pandemic was a ‘quiet killer.’ Ten years after swine flu, no one can predict the next one. STAT, Health. From https://www.statnews.com/2019/06/11/h1n1-swine-flu-10-years-later/ ↵
- Osterholm, MT., Kelley, NS., Manske, JM., Ballering, KS., Leighton, TR. (October 2012). CIDRAP Comprehensive Influenza Vaccine Initiative report. University of Minnesota, Academic Health Center. From https://www.cidrap.umn.edu/sites/default/files/public/downloads/ccivi_report.pdf ↵
- Tagliabue,F.,Galassi,L., Mariani,P.(2020). The “Pandemic” of Disinformation in COVID-19. SN Comprehensive Clinical Medicine, 2 (9),1287. From https://doi.org/10.1007/s42399-020-00439-1 ↵
- Grimes, DR. (March 12, 2021). Medical disinformation and the unviable nature of COVID-19 conspiracy theories. PLOS One (Pone). From https://doi.org/10.1371/journal.pone.0245900 ↵
- Dunleavy, Daniel, & Hendricks, Vincent. (2020, September 28). Fast Science, Slow Science: Finding Balance in the Time of COVID-19 and the Age of Misinformation (Version 1). Zenodo. http://doi.org/10.5281/zenodo.4056909 ↵
- Smriti Mallapaty, S. (28 January 2022). Where did Omicron come from? Three key theories The highly transmissible variant emerged with a host of unusual mutations. Now scientists are trying to work out how it evolved. Nature. From https://www.nature.com/articles/d41586-022-00215-2 ↵
- Haidong Wang, H., Paulson, KR., Pease, SA., Watson, S. et al. (April 16, 2022). Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet, 399 (10334), 1513. From https://doi.org/10.1016/S0140-6736(21)02796-3 ↵
- No author. (No date). Johns Hopkins University Coronavirus Resource Center. From https://coronavirus.jhu.edu/map.html ↵
- aidong Wang, H., Paulson, KR., Pease, SA., Watson, S. et al. (April 16, 2022). Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet, 399 (10334), 1513. From https://doi.org/10.1016/S0140-6736(21)02796-3 ↵
- CDC. (n.d.). Vaccines for Your Children, Diseases & the Vaccines that Prevent Them. From https://www.cdc.gov/vaccines/parents/diseases/index.html ↵
- World Health Organization. (2020). How do vaccines work? From https://www.who.int/news-room/feature-stories/detail/how-do-vaccines-work ↵
- Excler, JL., Saville, M., Berkley, S. et al. (2021). Vaccine development for emerging infectious diseases. Nat Med 27, 591–600. From https://www.nature.com/articles/s41591-021-01301-0 ↵
- CDC. (no date). Show Me the Science - Why Wash Your Hands? From https://www.cdc.gov/handwashing/why-handwashing.html ↵
- Goldust, M., Abdelmaksoud, A., & Navarini, A. A. (2020). Hand disinfection in the combat against COVID-19. Journal of the European Academy of Dermatology and Venereology : JEADV, 34(9), e454–e455. https://doi.org/10.1111/jdv.16574 ↵
- CDC. (2022). How to Protect Yourself & Others. From https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html ↵
- Tabatabaeizadeh S. A. (2021). Airborne transmission of COVID-19 and the role of face mask to prevent it: a systematic review and meta-analysis. European journal of medical research, 26(1), 1. https://doi.org/10.1186/s40001-020-00475-6 ↵
- CDC. (no date). History of Quarantine. From https://www.cdc.gov/quarantine/historyquarantine.html ↵
- Kiliç, R., Ataman Hatipoğlu, Ç., & Güneş, C. (2020). Quarantine and its legal dimension. Turkish journal of medical sciences, 50(SI-1), 544–548. https://doi.org/10.3906/sag-2004-153 ↵
- CDC. (no date). Quarantine and Isolation. From https://www.cdc.gov/quarantine/index.html ↵
- CDC. (No date). Isolation. From https://www.cdc.gov/coronavirus/2019-ncov/your-health/quarantine-isolation.html#iso ↵
- Barbisch, D., Koenig, K. L., & Shih, F. Y. (2015). Is There a Case for Quarantine? Perspectives from SARS to Ebola. Disaster medicine and public health preparedness, 9(5), 547–553. https://doi.org/10.1017/dmp.2015.38 ↵
A distinct set of concepts or thought patterns, including theories, research methods, postulates, and standards for what constitute legitimate contributions to a field. It comes from the Greek word, "pattern", and is used to illustrate similar occurrences. From https://en.wikipedia.org/wiki/Paradigm
The term refers to individuals who have specialized training and who are the first to arrive and provide assistance or incident resolution at the scene of an emergency.
The acronym stands for Emergency Medical Technicians. Same as Paramedics.
The term refers to biological, chemical, radiological, and, nuclear agents used to kill or spread fear in populations.
Bio = refers to the use of biological weapons such as viruses, bacteria, or their toxins).
Terrorism = the intentional attack to use those biological agents for mass destruction.
The CDC defines bioterrorism as the intentional release or threat of release of biologic agents (i.e. viruses, bacteria, fungi or their toxins) in order to cause disease or death among human population or food crops and livestock to terrorize a civilian population or manipulate the government.
A substance that causes tissue blistering.
“Energy traveling through space. Some types of radiation associated with radioactivity are alpha and beta particles and gamma and X rays.”
the amount of money allowed for the public and health care system) (or, for the health of a nation) which in the U.S. is approximately 16% of the Gross Domestic Product (or, GDP).
[["Linking Core Functions of Public Health and EPHS","Core Functions of Public Health"," Essential Public Health Service (EPHS)","Activities (How?)"],["","Policy development\n","Inform, educate, and empower people about health issues.","Informing, educating, and empowering people about health issues "],["","","","Community development activities\n"],["","","","Social marketing and targeted media public communication"],["","","","Provision of accessible health information resources at community level"],["","","","Active collaboration with personal healthcare providers to reinforce health promotion messages and programs"],["","","","Joint health education programs with schools, churches, work sites, and others"],["","","Mobilizing community partnerships to identify and solve health problems","Convening and facilitating partnerships among groups and associations"],["","","","Undertaking defining health improvement planning process and health projects"],["","","","Building a coalition to draw on the full range of potential human and materials resources to improve community health"],["","","Developing policies and plans that support individual and community health","Leadership development at all levels of public health"],["","","","Systematic community level and state level planning for health improvement in all jurisdictions"],["","","",""],["","","",""]]