Main Body
5 Public Health System in the United States
Hector (Giovanni) Antunez
Learning Objectives
By the end of this chapter, the learner will be able to
The United States Health System
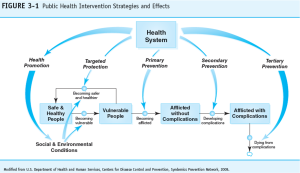
One of the major objectives of this chapter is to Learn about the programs and services that constitute what is known as the ‘public health system’ in the United States. In general, it is accepted that the health system includes public health because of the importance of prevention, but the Health System in the United States is highly focused on healthcare services that are mostly curative) and that requires about $4.3 trillion or $12,914 per person in 2022 (In the context of the nation’s Gross Domestic Product (GDP), health spending accounted for 18.3%). [1]. As said before, one of the difficulties in the health care system in the U.S. is that prevention is not always part of the “health services” provided to people but since there is an important distinction between curative and preventive health care, the following terms need to be reviewed for a better understanding of the content of this chapter, and related overall content of the book.
Understanding Prevention and Health Services in the U.S.
 |
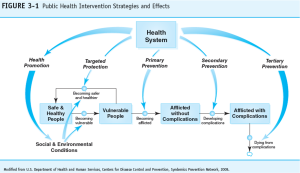
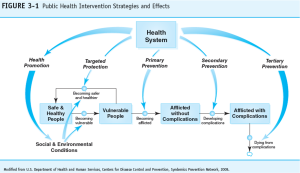
This type of approach is called, a syndemic approach to public health problems, which should help to find/create the solutions.[2] As briefly mentioned before, the idea is that these ‘health strategies’ that can be used as markers, and tools that can assist in the outcome’s evaluation of services. So, interventions can be evaluated and improved based on the results of those evaluations.
In general, the term refers to activities that attempt to modify human behaviors to reduce those known to affect adversely the ability to resist disease, or, injury-inducing factors, thereby eliminating exposures to harmful factors. Or, as the World Health Organization (WHO) defines the term, Health promotion is “[T]he process of empowering people to increase control over their health and its determinants through health literacy efforts and multisectoral action to increase healthy behaviors.”[3]
 |
| Health Promotion (Word Cloud). Find source later. To see details of the image including content, right click and choose, open image in new tab. |
In general, it can be considered as part of health promotion. Health protection refers to specific protection activities that provide individuals with resistance to factors (such as bacteria and viruses) or modify environments to decrease potentially harmful interactions of health-influencing factors (such as toxic exposures in the workplace).
 |
| Health Protection. Find source info later. |
Examples of health protection include the use of seat belts while driving and using helmets at work to protect from some environmental exposures or injuries. The use of vaccines is another common example of health protection, and preventive treatment with antibiotics for example in the case of family members exposed to tuberculosis but who had not present symptoms of the disease, or who don’t have active tuberculosis.
The next set of conceptual definitions includes, ‘early case finding and prompt treatment’, ‘disability limitation’, and ‘rehabilitation’.
Early Case Finding and Prompt Treatment, Disability Limitation, and Rehabilitation
If looking in detail back to the definition of health promotion and health (or, specific) protection, the focus of both is in the healthy state, when no disease is affecting the person. But since there is also the existence of disease/injury, a series of health strategies and activities are needed to manage those situations. These strategies and activities are those that facilitate the early detection (or, case identification), immediate/prompt treatment, and rehabilitation if the person survives the disease or, injury without dying. [4]
Early Detection and Case Finding
The strategy that is commonly used for “Early detection” is, screening. Examples of screening include, vision tests, mammograms, pap smear (to detect early cases of cervical cancer), etc.
How are the cases found?
If the definition of what constitutes a ‘case’ for a specific problem or, health issue is defined (a piece of information usually provided by medical textbooks or, directly from the Centers for Disease and Controls in the U.S.). The ‘case finding’ will be conducted by finding those individuals who meet the disease/condition criteria (detected frequently from the screening); once this is done, these become the ‘cases.
Prompt Treatment, Disability Limitation, and Rehabilitation
Thinking on a continuum and, after the cases are identified, the next step is the ‘ disease management‘ stage, which occurs after the individual’s diagnosis is established. A significant part of the disease management stage is the institution of treatment (or, not treatment in some cases), which can be prompt, or delayed. The results of the treatment depend on whether the treatment is effective and completed. Even though a person may receive and complete treatment for a disease or, health condition; disability may occur as a sequel to the main health problem, for example, the case of suffering a stroke in which the person loses some motor functions including speech problems. In this case, the most important intervention is to limit (make it worse) the limitation or teach the person how to function/live with it more effectively; these activities constitute the Rehabilitation stage, which is a common strategy used to limit disability.
Prevention and Health Services
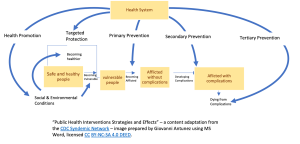
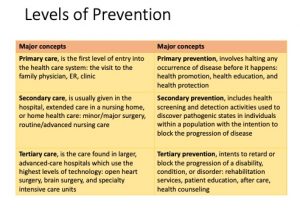
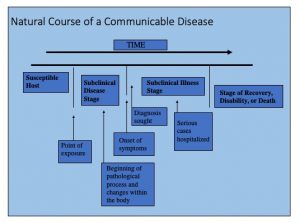
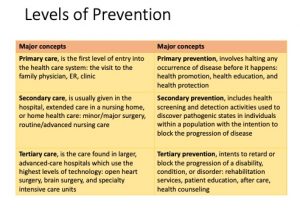
An additional set of interventions commonly used in health care include what is known as the “Levels of Prevention” strategies. These concepts have been developed using the concept of natural course of disease.
The natural course of a disease
From its beginning to end, each disease has a natural course (or, ‘natural history’). This can be observed if no medical intervention is taken, and the disease can run its full course. Although this concept is commonly found in an epidemiology textbook (see Chapter 1 in my epidemiology textbook for an extended version of this concept), it is presented here to provide a context to the information that can be useful for all kinds of public health professionals. The following image summarizes (and, outlines) the main components of the natural history of disease.
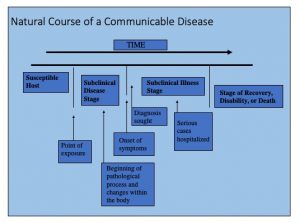 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
This model (of natural history of disease) has been used to develop the concepts of primary, secondary, and tertiary prevention that is commonly used in medicine, public health, and especially in public health education. Please note that the model applies mainly to the study of infectious, or, communicable diseases, it does not help much in the study of non-communicable (or, non-infectious) diseases.
The susceptible host matches the majority of situations known as primary prevention, primary prevention which is composed of a series of interventions, mainly medical and public health actions that help to prevent diseases.
Examples of Primary Prevention include the use of pap smears to prevent and detect early stages of cervical cancer, mammograms, digital rectal exams, colonoscopies, and other common screening tests. The idea is to identify the risk, of the disease in an early stage mostly before symptoms develop.
Secondary Prevention is the most expensive stage because the cases that are serious or, need intense treatment are hospitalized to receive a more intensive intervention, those cases that are not hospitalized are usually given treatment under supervision, especially for middle cases of a disease. In the secondary prevention step, the person recovers or dies. If the person survives and becomes disabled, then, the individual enters the tertiary level of prevention, which is next.
This phase is commonly misunderstood because many people see rehabilitation as part of the secondary prevention in which only medical care professionals provide services to rehabilitate the affected individual, but in general, going beyond the medical model, rehabilitation is more than just medical care, many times it means, helping the affected individual to improve the quality of life and to come back to society in a productive manner.
In addition, the following table provides additional details including examples that should help to understand the above-mentioned concepts:
 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
The levels of prevention can be linked to the clinical model, and this helps to put into context the common medical and public health interventions that most people use to be seen as part of the work of the medical and public health work. See a summary of this comparison in the following table:
| In the clinical model, there are three levels of health care services | In the public health model, there are three level of prevention |
| Primary care | Primary prevention |
| Secondary care | Secondary prevention |
| Tertiary care | Tertiary prevention |
Updates to the classic levels of prevention
The above information about the levels of prevention is the most common classification, however, two more levels have been added in recent decades, the first is, primordial prevention – before primary prevention, and quarternary prevention – after tertiary prevention.[5]
Primordial Prevention, it refers to the strategies used before primary prevention, for example, changes or aspects related to the “Built Environment”: Access to safe walking paths; access to stores with healthy food options. Also, changes in “Government policies” such as increasing taxes on cigarettes; decreasing advertisement of tobacco.[6]
On the other hand, is the concept of Quarternary prevention, it refers to strategies after tertiary prevention, examples include, several conditions that are the result of over medicating or those conditions susceptible to overtreatment, the following is a list of these conditions: use of hormone replacement therapy led to an increased number of cases of breast cancer, stroke, and thromboembolic events; medically unexplained symptoms; use of antiarrhythmic drugs after myocardial infarction that reduced arrhythmias but increased mortality; radiological incidental melanomas; functional disorders and, bodily distress syndrome. [7]
Important comments about the information above
The above distinctions should help public health professionals in training, especially health educators to better understand the differences between the levels of care and the level of prevention, especially for students who are not familiar with the United States healthcare system. This system works differently in other parts of the world, especially in developing countries. So, the comparison should also help to conciliate the differences.
Applying the content…
Using the concepts reviewed so far in this textbook, do the following:
1. Name a health problem (for example, new HIV infections in the U.S., Opioid Use, etc.).
2. Describe interventions for the health problem that you have identified:
The Health System in the United States
As mentioned earlier in this chapter, the healthcare system in the United States was a $4.3 trillion industry in the year 2022. I used the term “business” to refer to this system, even though some people may not prefer it as the system is primarily intended to serve people. [8] a review of the information (mainly numerical data) will be presented to give the reader an overall picture of the current situation of the health care system in the U.S. and its people.
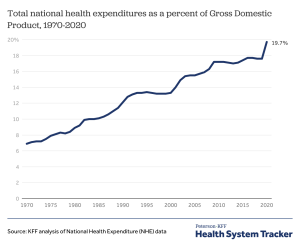
Recall - The National Health Expenditure
In the U.S., How much of the Gross Domestic Product (GDP) is spent on health? Since this topic has been covered in the previous chapter. For now, the content that follows will cover some content related to how the national healthcare expenditure is used.
|
"Total National Health Expenditure", Health System Tracker, Public Domain. |
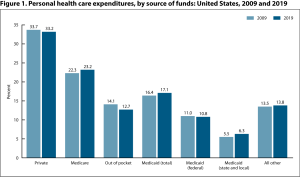
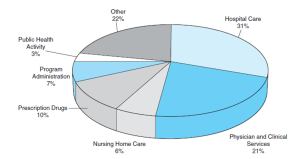
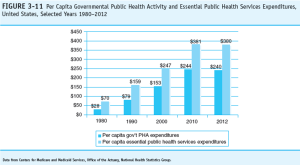
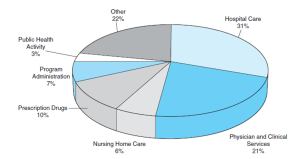
How much of the National health expenditure is assigned for health care services? Or, what is the budget's distribution? The answer to this question has been also provided in previous chapter. But here an update is presented in the following image provided by a report from the American Medical Association (AMA).
 |
|
“Health care spending explained,” image from the American Medical Association (AMA). Public domain.
|
The expending is distributed in the following services:[9]
- Hospital care
- Physician services
- Clinical services
- Prescription drugs
- Nursing care facilities
- Home health care
- Other personal health care costs
- Government administration: includes all administrative costs associated with insuring individuals in health insurance programs
- Net cost of health insurance: The difference between what insurers incur in premiums and the amount paid in benefits. This includes administrative costs, additions to reserves, rate credits and dividends, premium taxes and fees, and net underwriting gains or losses
- Government public health activities
- Investment spending
National Health care utilization
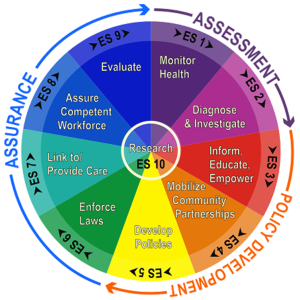
It is crucial to review the services offered by the public health system in the United States, given the allocated budget for it. In this context, the question is, what are the public health services offered in the United States? The section starts with a revision of what is know as the Essential Public Health Services explained in detail in the following paragraphs.
Essential Public Health Services (EPHS)
The following are the public health services that are considered essential, from these other subprograms derive.
1.Monitor health status to identify community health problems.
2. Diagnose and investigate health problems and health hazards in the community.
3. Inform, educate, and empower people about health issues.
4. Mobilize community partnerships to identify and solve health problems.
5. Develop policies and plans that support individual and community health efforts.
6. Enforce laws and regulations that protect health and ensure safety.
7. Link people to needed personal health services and assure the provision of health care when otherwise unavailable.
8. Assure a competent public health and personal health care workforce.
9. Evaluate effectiveness, accessibility, and quality of personal and population-based health services.
In a graphic form, the EPHS are represented in a wheel of services:
 |
| "Original Essential Public Health Services (EPHS) wheel", image from CDC. Public domain. |
This graphic also presents, the three core functions of public health: Assurance, Assessment and Policy Development. This topic which will be developed in detail in one of the upcoming chapters in the book.
The U.S. Health care system: Demographics, Disease and Utilization Trend
In the United States, the changes in demographics also known as "demographic shifts" is having an impact in the utilization of health care services, including public health services. What are these changes? One is the aging of the population, more and more the number of people aged 65 and older is growing, at the point that it is projected that the number of over 65 will double from 52 million in 2018 to 95 million by 2060 (in terms of total population share, the 65 and older group will increase from 16% to 23%.[10]
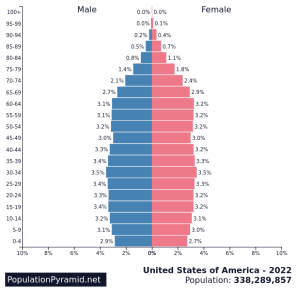
"Population Pyramid of the United States", image from PopulationPyramidNet, No license stated. |
It is also important to note that this older population is overall, more diverse in term of race and ethnicity, example is found in another projection, which is that between 2018 and 2010, the older non-Hispanic white population will drop from 77% to 55%. Although the increased diversity among the older population which could be considered a positive, the reality is that the gap between the older and the young populations is increasing, those individuals under age 18 are more rapidly becoming racial and ethnically diverse making the separation between older adults and young individuals more accentuated, this is called, the "diversity gap".[11]
Trends in terms of disease
If people are living longer, then, chronic diseases became the norm for the elder population, and these diseases are related to two main factors among others, obesity and tobacco use (at the present, but mostly in the past during their young age). As the president and CEO of the Association of American Medical Colleges (AAMC) said: “The nation’s population is growing and aging, and as we continue to address population health goals like reducing obesity and tobacco use, more Americans will live longer lives. These factors and others mean we will need more doctors..."[13]
What is the importance of the above-mentioned trends? It means that in terms of health care services, the demand will be focused more on those two major groups, the very young population and the group of older adults who will be highly diverse putting more demand on services that should be more culturally appropriate in terms of language and culture, just two mention two major need among diverse populations in the United States. Also, if the U.S. population is aging is because people in the U.S. are living longer (greater life expectancy as reviewed before in this chapter), and more chronic diseases associated with obesity and tobacco use will be in demand for treatment and control at the level of the healthcare system and services, which also mean that more physicians and nurses will be needed soon to respond to these needs.
Resources in Healthcare: health care providers
Another important area of the public healthcare system is the supply of healthcare resources, how much is available for the consumer, and how much is affordable for the population? One important element related to the resources in healthcare is the number of healthcare providers such as physicians and nurses available for the care of the population. The current numbers and projections of the number of physicians and nurses in the U.S. healthcare system show a shortage. See some of the numbers presented in the images below – the first, is for physicians and the second image is for nurses.
 |
| "National Physician Shortage," Image from pbs media, no license stated. |
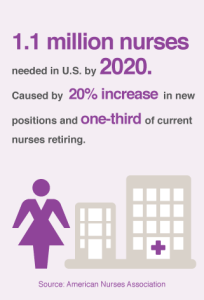 |
| "1.1 million nurses needed in U.S. by 2020," Image from healthline.com, no license stated. |
Physicians: Contradictory numbers
Physicians in the U.S. had increased in number from two sources: 1) the number of medical graduates from U.S. medical schools had increased in recent years [but not enough to cover the needs of the population] and, 2) the constant flow of foreign graduates’ physicians that have immigrated to the U.S., and obtained a license to practice in the U.S. That said, this information is contradictory, because as the graphs have shown above, the number of physicians in the U.S. shows a shortage, and the explanation is that there will not be enough physicians for the projected growth of the population in the next decades. An additional reason for the decline in the number of physicians in the U.S. is that a great number of current practitioners will be retiring soon, with no immediate replacement from the graduate medical schools or, the international flow of foreign graduates who obtained their license to practice medicine in the United States. An additional problem among the physician population that it is important to note also is that most physicians prefer to work on specialties making the generalist and the family care professional less in terms of numbers, primary care physicians had not increased in recent decades, creating a gap between specialist services and family practice, although the country needs more primary care providers. [14]
Nurses: more are needed
The shortage of nurses is very similar to the one discussed above about the number of physicians in the U.S., but there is one great difference, no matter how many nurses could come from abroad and get licensed in the U.S., augmented with the number of nurses graduated from U.S. nurses' schools, the shortage of nurses, faculty to train nurses and resource still be great. There is a need for more nurses in the country. [15]
Other healthcare professionals
The healthcare system
The four components of a healthcare system
At the same time, it is accepted that the following are the components of a health care delivery system: financing, insurance, delivery and payment; in some cases, reimbursement is also included instead of payment. Together these functional components make up what is known as the quad-function model.
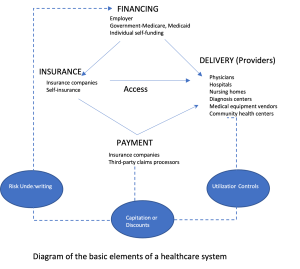 |
| Image prepared by Giovanni Antunez using MS Word, Licensed CC BY 4.0 |
Let's look at the functions independently, first, financing, what is it? Essentially financing is the act of providing money for a service or providing financial funds in difficult situations. Patients/clients can pay for health care in different form being the most common: out of pocket, paying by using a group/individual health insurance, or using a plan financed by the government. Second, insurance, which in general can be obtained from the work-place or the federal government, most of the time, insurance are bought it from private insurance companies. Third, delivery, this part of the health system can take many forms depending of the overall structure of the system - this topic will be covered in more details in the following paragraphs of this section. Fourth, payment, this component usually refers to those services covered by private insurances companies, government plans or out of pocket for consumers.
Delivery of Services, what are they? Examples
What is a delivery service? One definition states, "A health care delivery system is an organization that provides resources and treatments that help people when they are sick or injured, and helps them stay healthy through preventive care." [18] So, it is the organization, and it is also the model (which will be discussed here in this section later). In general, it is accepted that the following are the most common health delivery systems: [19]
- Exclusive Provider Organization (EPO)
An EPOs refers to a network of providers who have agreed to provide care for the members at a discounted rate, or, through sliding fees. - Health Maintenance Organization (HMO)
HMO’s often use the Primary Care Physician (PCP) as the “gatekeeper”. A patient receives all primary and preventative care from the PCP. Any care needs outside the PCP’s scope of practice would be referred out and coordinated by the PCP. Any care, other than emergency care, not coordinated through the PCP would not be covered by the HMO.In general, there four types of HMOs- Group Model HMOs
- Individual Practice Association (IPA) Model HMO
- Network Model HMO
- Staff Model HMO
- Integrated delivery system (IDS)
IDS’s are systems of healthcare that provide services across the continuum of care settings. Providers including physicians and hospitals are often owned or aligned with an insurance company. Some of the services provided include primary care, hospital, outpatient, home health and rehabilitation. - Preferred Provider Organization (PPO)
PPO’s contract with providers to dispense care at a discounted rate. The providers with whom they contract are considered “network providers or prefered providers”. If the patient uses a provider that is not part of the network they will have a larger financial responsibility. - Point-of-Service (POS) Plan
The Point-of-Service Plan is a combination of a PPO and HMO. The patient can choose to receive care in network at little or no cost, or to go out of network and have larger out of pocket expenses.
Use of Care: Overuse and Underused in the U.S. health system
In addition to those major demographic changes, there is always a question about the use of health care services, and one of these questions is: from those using the system, which one is the major problem, overuse, or underused care? Contrary to what most people think, underused of care is a greater problem than overuse, how is this possible? Let's look at the research on the topic and the appropriate definitions of the term to help us understand this situation. First, what is overuse? Practically, overuse can occur for example when a drug or treatment is given without medical justification. It includes treating people with antibiotics for simple infections – or failing to follow effective options that cost less or cause fewer side effects. Secondly, the term, underused? Underused happens for example when doctors or hospitals neglect to give patients medically necessary care or to follow proven health care practices – this happens a lot among many diabetic patients who don’t receive the right evidence-based care for such chronic conditions such as high blood pressure, diabetes, and heart disease. Third, another term that is not commonly heard of is the term, misuse. Misuse which is another way of describing medical errors frequently occurs for example, when a patient doesn’t fully benefit from a treatment because of a preventable problem – or when a patient is harmed by a treatment. [20] The literature reports that between 44,000 and 98,000 people die annually from preventable errors. [21] Especially for those people who are afraid about the overuse of the system as it was mentioned at the beginning of this section, contrary to what most people think, underused of care is a greater problem than overuse. [22]
To think about...
After reading about the use of health services and the terms, overuse, underused, and misuse, what do you think are the main reasons for each one of these categories, make a list of these reasons and discuss/share your answers in a small group with your classmates.
In summary, this chapter had covered (in a panoramic view) essential elements of the Public Health System in the United States. Additional concepts not covered in this chapter will be developed in the upcoming content in the book.
- Centers for Medicare and Medicaid Services (CMS). (Dec. 15, 2022). National Health Expenditure Data, Historical section. From https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical ↵
- The Lancet [Editorial]. (March 4, 2017). Syndemics: health in context. The Lancet, 389, 881. From DOI:https://doi.org/10.1016/S0140-6736(17)30640-2 ↵
- World Health Organization (WHO). (n.d.). Health promotion and disease prevention through population-based interventions, including action to address social determinants and health inequity. Operational definition. From https://www.emro.who.int/about-who/public-health-functions/health-promotion-disease-prevention.html ↵
- Minnesota Department of Health. (2019). Public health interventions: Applications for public health nursing practice (2nd ed.). From https://www.health.state.mn.us/communities/practice/research/phncouncil/docs/PHInterventions.pdf ↵
- Kisling LA, M Das J. Prevention Strategies. [Updated 2023 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537222/ ↵
- Fielding, R., Chee, Y. Y., Choi, K. M., Chu, T. K., Kato, K., Lam, S. K., Sin, K. L., Tang, K. T., Wong, H. M., & Wong, K. M. (2004). Declines in tobacco brand recognition and ever-smoking rates among young children following restrictions on tobacco advertisements in Hong Kong. Journal of public health (Oxford, England), 26(1), 24–30. https://doi.org/10.1093/pubmed/fdh118 ↵
- References about these examples can be found at Kisling LA, M Das J. Prevention Strategies. [Updated 2023 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537222/ ↵
- Centers for Medicare and Medicaid Services (CMS). (Dec. 15, 2022). National Health Expenditure Data, Historical section. From https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical[/footnote]. This health system is expected to cover and respond to the needs of a nation that has a population of 333,287,557 million people, [footnote]National Bureau of Census. (Dec. 22, 2022). United States population estimates. From https://www.census.gov/newsroom/press-releases/2022/2022-population-estimates.html[/footnote] a great number of whom are over the age of 65. Add to this the fact that the healthcare system must respond to an increasing number of ethnically and racially diverse groups seeking healthcare services. These two mentioned elements are enough to overwhelm a system that does not have all the resources for preventive and curative health, or the resources are insufficient. In this context and using the Health of the U.S. report from the CDC. [footnote] CDC. (n.d.). Health in the U.S., National Center for Health Statistics. From https://www.cdc.gov/nchs/hus/index.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fnchs%2Fhus.htm ↵
- American Medical Association (AMA). (2023). Trends in health care spending. From https://www.ama-assn.org/about/research/trends-health-care-spending ↵
- U.S. Census Bureau. (2021). 2017 National Population Projections Tables: Main Series. Population Projections. From https://www.census.gov/programs-surveys/popproj.html ↵
- U.S. Census Bureau. (2021). Projections of race and Hispanic origin, tables 4-7. Population Projections. From https://www.census.gov/programs-surveys/popproj.html ↵
- National Bureau of Census. (Dec. 22, 2022). Population projections. Video From https://www.census.gov/programs-surveys/popproj.html ↵
- Finnegan, J. (April 23, 2019). Physician shortage: The numbers keep climbing, now estimated at 122,000 by 2032. Fierce Health Care. From https://www.fiercehealthcare.com/practices/physician-shortage-numbers-keep-climbing-now-estimated-at-122k-by-2032 Also, a full report is available in pdf, link is here. ↵
- Association of American Medical Colleges (AAMC). (June 11, 2021). AAMC Report Reinforces Mounting Physician Shortage. From https://www.aamc.org/news-insights/press-releases/aamc-report-reinforces-mounting-physician-shortage ↵
- Hamlin, K. (March 21, 2023). Why Is There a Nursing Shortage? Nurse Journal. From https://nursejournal.org/articles/why-is-there-a-nursing-shortage/ ↵
- Manyazewal T. (2017). Using the World Health Organization health system building blocks through survey of healthcare professionals to determine the performance of public healthcare facilities. Archives of public health = Archives belges de sante publique, 75, 50. https://doi.org/10.1186/s13690-017-0221-9 ↵
- Definition of a health system found at the: Agency for Health Care Research and Quality (AHQR). (n.d.). NBER Center of Excellence’s Definition of a Health System. From https://www.ahrq.gov/chsp/defining-health-systems/index.html#:~:text=The%20National%20Bureau%20of%20Economic,a%20form%20of%20joint%20management). ↵
- Topper, A. (2022). What is a Health Care Delivery System? Compare and Contrast Health the US Healthcare Delivery System with Other Industrialized Countries. From https://study.com/learn/lesson/health-care-delivery-system-concept-components-types.html ↵
- No author. (n.d.). Healthcare delivery systems. Case Management Study Guide. From https://casemanagementstudyguide.com/ccm-knowledge-domains/healthcare-management-delivery/healthcare-delivery-systems/ ↵
- The National Partnership for Women & Families. (2009). Overuse, Underused and Misuse of Medical Care, Fact Sheet. From www.nationalpartnership.org ↵
- Institute of Medicine (US) Committee on Quality of Health Care in America, Kohn, L. T., Corrigan, J. M., & Donaldson, M. S. (Eds.). (2000). To Err is Human: Building a Safer Health System. National Academies Press (US). From https://pubmed.ncbi.nlm.nih.gov/25077248/ ↵
- Sullivan, JD. (Oct. 6, 2016). Underused is Rampant, But Overuse is All We Talk About. From https://thehealthcareblog.com/blog/2016/10/06/underuse-is-rampant-but-overuse-is-all-we-talk-about/ ↵
although this term is related to 'health indicators' the term here refers mostly to a series of 'tools' that are used in prevention.
Syndemic(s) is a conceptual framework for understanding diseases or health conditions that arise in populations and that are exacerbated by the social, economic, environmental, and political milieu in which a population is immersed.
a strategy (usually, screening - see definition later) used to detect the early presence of a disease such as cancer and other non infectious, or, infections' diseases.
an epidemiological strategy used to separate those who are sick for those who are not using a test. Example, screening for tuberculosis will provide information about those persons who are positive or, not to the tuberculin skin test. Those found positive in the test will follow additional clinical procedures and test to confirm (or, not confirm) that the person is infected or, not with tuberculosis.
In this context, it refers to the individuals who meet the clinical criteria [already established] for a disease or, any other health problem.
This chapter is more about how the public health system is organized in the U.S. mostly chapter 3 in Turnock's book
Learning Objectives
By the end of this chapter, the learner will be able to
-
Learn about the programs and services that constitute what is known as the 'public health system' in the United States
- Learn about importance of public health programs and services in the U.S.
- Learn about the structure/components of the public health programs and services in the U.S.
- List the major assessment tools used to evaluate the proper functioning, and efficiency of most common public health program and services
- Link the public health program and services with the Healthy People 2030 Objectives and identify its commonalities
- Provide examples of successful public health program and services in the U.S. by identifying those elements that make these programs successful
Chapters' overview -
The United States Health System
One of the major objectives of this chapters is to Learn about the programs and services that constitute what is known as the 'public health system' in the United States. In general, it is accepted that the health system includes public health because of the importance of prevention, but in reality, the Health System in the United States is highly focused on health care services that are mostly curative) and that require about $4.3 trillion or $12,914 per person in 2022 (In the context of the nation's Gross Domestic Product (GDP), health spending accounted for 18.3%).[1]. As said before, one of the difficulties in the health care system in the U.S. is that prevention is not always part of the "health services" provided to people but since there is an important distinction between curative and preventive health care, the following terms need to be reviewed for a better understanding of the content of this chapter, and related overall content of the book.
Understanding Prevention and Health Services in the U.S.
 |
| Make my own or, find the source - which I could not find it yet as Dec. 27, 2022 |
In general, the term refers to activities that attempt to modify human behaviors to reduce those known to affect adversely the ability to resist disease, or, injury-inducing factors, thereby eliminating exposures to harmful factors. Or, as the World Health Organization (WHO) defines the term, Health promotion is "[T]he process of empowering people to increase control over their health and its determinants through health literacy efforts and multisectoral action to increase healthy behaviors."[3]
 |
| Health Promotion (Word Cloud). Find source later. To see details of the image including content, right click and choose, open image in new tab. |
Examples of health promotion include: activities for the community-at-large or for populations at increased risk of negative health outcomes. Health promotion usually addresses behavioral risk factors such as tobacco use, obesity, diet and physical inactivity, as well as the areas of mental health, injury prevention, drug abuse control, alcohol control, health behavior related to HIV, and sexual health.
In general, it can be considered as part of health promotion. Health protection refers to specific protection activities that provide individuals with resistance to factors (such as bacteria and viruses), or, modify environments to decrease potentially harmful interactions of health influencing factors (such as toxic exposures in the workplace).
 |
| Health Protection. Find source info later. |
Examples of health protection include the use of seat belts while driving, using helmets at work to protect for some environmental exposures, or, injuries. The use of vaccines is another common example of health protection, and preventive treatment with antibiotics for example in the case of family members exposed to tuberculosis but who had not present symptoms of the disease, or, who don't have active tuberculosis.
Early Case Finding and Prompt Treatment, Disability Limitation, and Rehabilitation
Early Detection and Case Finding
How are the cases found? Assuming that the definition of what constitute a 'case' for a specific problem or, health issue is defined (an information usually provided by medical textbooks or, directly from the Centers for Disease and Controls in the U.S.). The 'case finding' will be conducted by finding those individual who meet the disease/condition criteria (detected frequently from the screening); once this is done, these became the ‘cases.
Prompt Treatment, Disability Limitation, and Rehabilitation
From its beginning to end, each disease has a natural course (or, 'natural history'). This can be observed if no medical intervention is taken and the disease is allowed to run its full course. Although this concept is commonly found in an epidemiology textbook (see chapter 1 in my epidemiology textbook for an extended version of this concept), it is presented here in order to provide a context to the information that can be useful for all kinds of public health professionals. The following image summarizes (and, outlines) the main components of the natural history of disease.
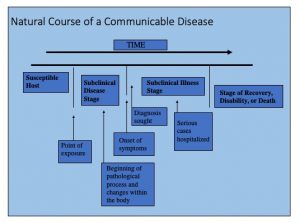 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
This model (of natural history of disease) has been used to develop the concepts of primary, secondary and tertiary prevention that is commonly used in medicine, public health and especially in public health education. Please note that the model applies mainly to the study of infectious, or, communicable diseases, it does not help much in the study of non-communicable (or, non-infectious) diseases.
Examples of Primary Prevention include, the use of pap smear to prevent and detect early stages of cervical cancer, mammograms, digital rectal exams, colonoscopies, and other common screening tests. The idea is to identify the risk, or, the disease in an early stage mostly before symptoms develop.
Secondary Prevention is the most expensive stage because the cases that are serious or, need intense treatment are hospitalized to receive a more intensive intervention, those cases that are not hospitalized are usually given treatment under supervision especially for middle cases of a disease. In the secondary prevention step, the person recovers or die. If the person survives and became disabled, then, the individual enters the tertiary level of prevention, which is next.
This phase is commonly misunderstood because many people see rehabilitation as part of the secondary prevention in which only medical care professionals provide services to rehabilitate the affected individual, but in general, going beyond the medical model, rehabilitation is more than just medical care, many times it means, helping the affected individual to improve the quality of life and to come back to society in a productive manner.
In addition, the following table provides additional details including examples that should help to understand the above mentioned concepts:
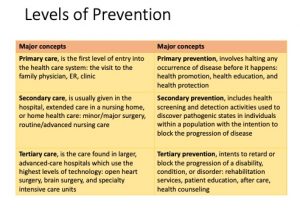 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
The levels of prevention can be linked to the clinical model, and this helps to put into context the common medical and public health interventions that most people are used to be seen as part of the work of the medical and public health work. See a summary of this comparison in the following table:
| In the clinical model, there are three levels of health care services | In the public health model, there are three level of prevention |
| Primary care | Primary prevention |
| Secondary care | Secondary prevention |
| Tertiary care | Tertiary prevention |
Important comments about the information above
The above distinctions should help public health professionals in training, especially health educators to better understand the differences between the levels of care and the level of prevention, especially for students who are not familiar with the United States healthcare system. This system works differently in other parts of the world, especially in developing countries. So, the comparison should also help to conciliate the differences.
Applying the content...
Using the concepts reviewed so far in this textbook, do the following:
1. Name a health problem (for example, new HIV infections in the U.S., Opioid Use, etc.
2. Describe interventions for the health problem that you have identified:
The Health System in the United States
As mentioned at the beginning of this chapter, in the year 2022, the health system in the U.S. is a $4.3 trillion business (I am using here the word, 'business' although some people don't like to use it when referring to a system that is created to serve people). [5]. This health system is expected to cover and respond to the needs of a nation that has a population of 333,287,557 million people, [6]in which a great number of them are over the age of 65. Add to this picture is the fact that the response of this system has to be designed in a way that respond to a growing number of ethnic and racial diverse group of people seeking health care services. These two mentioned elements are enough to overwhelmed a system that does not have all of the resources for preventive and curative health, or, the resources are insufficient. In this context and using the Health of the U.S. report from CDC,[7] a review of the information (mainly numerical data) will be presented with the purpose of giving the reader an overall picture of the current situation of the health care system in the U.S. and its people.
National Health expenditure
In the U.S., How much of the Gross Domestic Product (GDP) is spend in health?
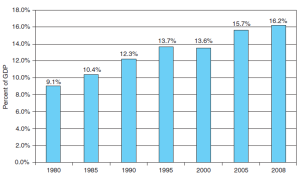 Percent of US National Gross Domestic Expenditures Spent for Health-Related Purposes, Selected Years, 1980-2008 Percent of US National Gross Domestic Expenditures Spent for Health-Related Purposes, Selected Years, 1980-2008 |
| Text Figure 3-6. Source: Data from Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group; U.S. Department of Commerce, Bureau of Economic Analysis.
Find new data - New data entered Dec-31-22 below
"Total National Health Expenditure", Health System Tracker, Public Domain. |
How much of the National health expenditure is for public health? Or, what is the budget's distribution?
 |
| update later
"Total National Health Expenditure", Health System Tracker, Public Domain.
"Personal Healthcare expenditures y source of funds", Centers for Medicare & Medicaid Services, National Health Expenditures Accounts, Public domain. Keep source below just for future needs See Sources and Definitions, National Health Expenditure Accounts (NHEA) and Health, United States, 2020–2021 Table HExpPers. |
 |
| Text Figure 3-7. Source: Data from Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group.
Find new data - |
National Health care utilization
A great number of the health care system's budget in the U.S. is utilized to serve an aging and diverse population, representing a
Knowing how much is assigned for public health service, it is important to review what are the services offered by the public health system in the U.S.
Essential Public Health Services (EPHS)
The following are the public health services that are considered essential, from these other subprograms derive.
In a graphic form, the EPHS are represented in a wheel of services:
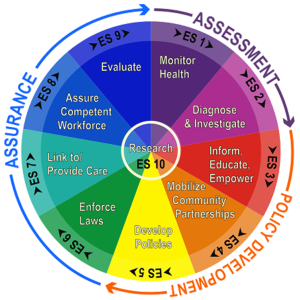 |
| Essential Public Health Services (EPHS) wheel |
These graphic representation also introduces the three major public health activities: Assurance, Assessment and Policy Development, which will be developed in content later [or, presented later also in another chapter, introduction to public health].
Public Health Activity and the Essential Public Health Services (EPHS)
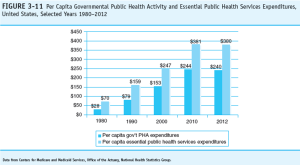
From the assigned budgetary expenditure, how much of the public health activity and EPHS is assigned and spent by government level? See graph:
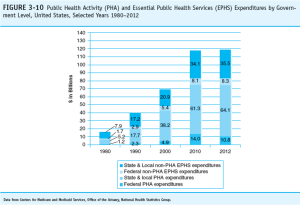 |
| Update this later |
Examine the web sites of these major health organizations: American Medical Association, American Hospital Association, American Nurses Association, and the American Association of Medical Colleges. Do your selections in the previous exercise differ from the priority issues of these organizations? How do you explain or account for any differences between the two lists?
“The nation’s population is growing and aging, and as we continue to address population health goals like reducing obesity and tobacco use, more Americans will live longer lives. These factors and others mean we will need more doctors,” Kirch said. https://www.fiercehealthcare.com/practices/physician-shortage-numbers-keep-climbing-now-estimated-at-122k-by-2032
What is the importance of the above mentioned trends? It means that in terms of health care services, the demand will be focused more on those two major groups, the very young population and the group of older adults who will be highly diverse putting more demand on services that should be more culturally appropriate in terms of language and culture, just two mention two major need among diverse populations in the United States. Also, if the U.S. population is aging is because people in the U.S. are living longer (greater life expectancy as reviewed before in this chapter) and also more chronic diseases associated with obesity and tobacco use will be on demand for treatment and control at the level of the healthcare system and services, which also mean that more physicians and nurses will be needed in the near future to respond to these needs
The next section is health care resources -
The role of the health care providers especially, physicians and nurses
Also, the role of insurance companies and its healthcare plans offered to the population.
Models (examples of delivery of services) as part of the resources.
Resources in Healthcare: health care providers
Another important area of the public health care system is the supply of health care resources, how much is available for the consumer, and how much is affordable for the population? One important element related to the resources in healthcare is the number of health care providers such as physicians and nurses available for the care of the population. The current numbers and projections of the number of physicians and nurses in the U.S. healthcare system show a shortage. See some of the numbers presented in the images below - first, for physicians and second image is for nurses.

Image link: https://pbs.twimg.com/media/D42KgM9W4AAZWMH?format=jpg&name=medium
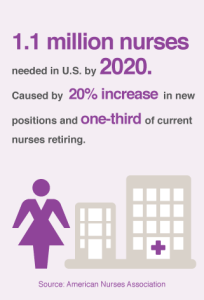
Image link: http://www.healthline.com/hlcmsresource/images/News/long-forms/nurses-1.png
Physicians: Contradictory numbers
Physicians in the U.S. had increased in number from two sources: 1) the number of medical graduates from U.S. medical schools had increased in recent years [but not enough to cover the needs of the population] and, 2) the constant flow of foreign graduates physicians that have immigrated to the U.S., and obtained a license to practice in the U.S. That said, this information is contradictory, because as the graphs have show above, the number of physicians in the U.S. show a shortage, and the explanation is that there will not be enough physicians for the projected grow of the population in the next decades. And, additional reason for the decline of the number of physicians in the U.S. in the near future is due to the fact that a great number of current practitioners will be retiring soon, with no immediate replacement from the graduate medical schools or, international flow of foreign graduated that obtained their license to practice medicine in the U.S.[10]
Nurses: more are needed
The shortage of nurses is very similar to the one discussed above about the number of physicians in the U.S., but there is one great difference, no matter how many nurses could come from abroad and get licensed in the U.S., augmented with the number of nurses graduated from U.S. nurses' schools, the shortage of nurses, faculty to train nurses and resource still be great. There is need for more nurses in the country.[11]
Other health care professionals
Laboratory and imaging technicians, Anesthesiologists, Pharmacists, Physical therapy, etc. these will be discussed in the next chapter about the US public health work force.
Trends in terms of disease
“The nation’s population is growing and aging, and as we continue to address population health goals like reducing obesity and tobacco use, more Americans will live longer lives. These factors and others mean we will need more doctors,” Kirch said. https://www.fiercehealthcare.com/practices/physician-shortage-numbers-keep-climbing-now-estimated-at-122k-by-2032
In the past decades, the number of physicians in the country had increased in recent years, this is not the same for the number of registered nurses that is experiencing a shortage, not only in terms of diversity but also in terms of numbers in general.
Physicians in the U.S. had increased in number (how many per inhabitant?) as part of the increased number of medical graduates from U.S. medical schools, but also for the greater numbers of foreign graduates that have immigrated to the U.S. and that are now practitioners in the U.S., without the intention to create confusion, the projected
it is important to note also that the majority of physicians prefer to work on specialties making the generalist and the family care professional less in terms of numbers, primary care physicians had not have increased in recent decades, creating a gap between specialist services and family practice, although the country needs more primary care providers. -- revise the terms, make sure is uniform, and find the data to support the statements.
health care practices – this happens a lot among many diabetic patients who don’t receive the right evidence-based care for such chronic conditions such as high blood pressure, diabetes and heart disease. Third, another terms that is not commonly heard of is the term, misuse? Misuse which is another way of describing medical errors frequently occurs for example, when a patient doesn’t fully benefit from a
treatment because of a preventable problem – or when a patient is harmed by a treatment. [12] The literature reports that between 44,000 and 98,000 people die annually from preventable errors.[13] Especially for those people who are afraid about overuse of the system as it was mentioned at the beginning of this section, contrary to what most people think, underused of care is actually a greater problem than overuse. [14]
After reading about use of health services and the terms, overuse, underused and misuse, what do you think are the main reasons for each one of the these categories, make a list of these reasons and discuss/share your answers in a small group with your classmates.
This chapter is more about how the public health system is organized in the U.S. mostly chapter 3 in Turnock's book
Learning Objectives
By the end of this chapter, the learner will be able to
-
Learn about the programs and services that constitute what is known as the 'public health system' in the United States
- Learn about importance of public health programs and services in the U.S.
- Learn about the structure/components of the public health programs and services in the U.S.
- List the major assessment tools used to evaluate the proper functioning, and efficiency of most common public health program and services
- Link the public health program and services with the Healthy People 2030 Objectives and identify its commonalities
- Provide examples of successful public health program and services in the U.S. by identifying those elements that make these programs successful
Chapters' overview -
The United States Health System
One of the major objectives of this chapters is to Learn about the programs and services that constitute what is known as the 'public health system' in the United States. In general, it is accepted that the health system includes public health because of the importance of prevention, but in reality, the Health System in the United States is highly focused on health care services that are mostly curative) and that require about $4.3 trillion or $12,914 per person in 2022 (In the context of the nation's Gross Domestic Product (GDP), health spending accounted for 18.3%).[15]. As said before, one of the difficulties in the health care system in the U.S. is that prevention is not always part of the "health services" provided to people but since there is an important distinction between curative and preventive health care, the following terms need to be reviewed for a better understanding of the content of this chapter, and related overall content of the book.
Understanding Prevention and Health Services in the U.S.
 |
| Make my own or, find the source - which I could not find it yet as Dec. 27, 2022 |
In general, the term refers to activities that attempt to modify human behaviors to reduce those known to affect adversely the ability to resist disease, or, injury-inducing factors, thereby eliminating exposures to harmful factors. Or, as the World Health Organization (WHO) defines the term, Health promotion is "[T]he process of empowering people to increase control over their health and its determinants through health literacy efforts and multisectoral action to increase healthy behaviors."[17]
 |
| Health Promotion (Word Cloud). Find source later. To see details of the image including content, right click and choose, open image in new tab. |
Examples of health promotion include: activities for the community-at-large or for populations at increased risk of negative health outcomes. Health promotion usually addresses behavioral risk factors such as tobacco use, obesity, diet and physical inactivity, as well as the areas of mental health, injury prevention, drug abuse control, alcohol control, health behavior related to HIV, and sexual health.
In general, it can be considered as part of health promotion. Health protection refers to specific protection activities that provide individuals with resistance to factors (such as bacteria and viruses), or, modify environments to decrease potentially harmful interactions of health influencing factors (such as toxic exposures in the workplace).
 |
| Health Protection. Find source info later. |
Examples of health protection include the use of seat belts while driving, using helmets at work to protect for some environmental exposures, or, injuries. The use of vaccines is another common example of health protection, and preventive treatment with antibiotics for example in the case of family members exposed to tuberculosis but who had not present symptoms of the disease, or, who don't have active tuberculosis.
Early Case Finding and Prompt Treatment, Disability Limitation, and Rehabilitation
Early Detection and Case Finding
How are the cases found? Assuming that the definition of what constitute a 'case' for a specific problem or, health issue is defined (an information usually provided by medical textbooks or, directly from the Centers for Disease and Controls in the U.S.). The 'case finding' will be conducted by finding those individual who meet the disease/condition criteria (detected frequently from the screening); once this is done, these became the ‘cases.
Prompt Treatment, Disability Limitation, and Rehabilitation
From its beginning to end, each disease has a natural course (or, 'natural history'). This can be observed if no medical intervention is taken and the disease is allowed to run its full course. Although this concept is commonly found in an epidemiology textbook (see chapter 1 in my epidemiology textbook for an extended version of this concept), it is presented here in order to provide a context to the information that can be useful for all kinds of public health professionals. The following image summarizes (and, outlines) the main components of the natural history of disease.
 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
This model (of natural history of disease) has been used to develop the concepts of primary, secondary and tertiary prevention that is commonly used in medicine, public health and especially in public health education. Please note that the model applies mainly to the study of infectious, or, communicable diseases, it does not help much in the study of non-communicable (or, non-infectious) diseases.
Examples of Primary Prevention include, the use of pap smear to prevent and detect early stages of cervical cancer, mammograms, digital rectal exams, colonoscopies, and other common screening tests. The idea is to identify the risk, or, the disease in an early stage mostly before symptoms develop.
Secondary Prevention is the most expensive stage because the cases that are serious or, need intense treatment are hospitalized to receive a more intensive intervention, those cases that are not hospitalized are usually given treatment under supervision especially for middle cases of a disease. In the secondary prevention step, the person recovers or die. If the person survives and became disabled, then, the individual enters the tertiary level of prevention, which is next.
This phase is commonly misunderstood because many people see rehabilitation as part of the secondary prevention in which only medical care professionals provide services to rehabilitate the affected individual, but in general, going beyond the medical model, rehabilitation is more than just medical care, many times it means, helping the affected individual to improve the quality of life and to come back to society in a productive manner.
In addition, the following table provides additional details including examples that should help to understand the above mentioned concepts:
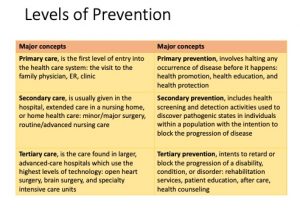 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
The levels of prevention can be linked to the clinical model, and this helps to put into context the common medical and public health interventions that most people are used to be seen as part of the work of the medical and public health work. See a summary of this comparison in the following table:
| In the clinical model, there are three levels of health care services | In the public health model, there are three level of prevention |
| Primary care | Primary prevention |
| Secondary care | Secondary prevention |
| Tertiary care | Tertiary prevention |
Important comments about the information above
The above distinctions should help public health professionals in training, especially health educators to better understand the differences between the levels of care and the level of prevention, especially for students who are not familiar with the United States healthcare system. This system works differently in other parts of the world, especially in developing countries. So, the comparison should also help to conciliate the differences.
Applying the content...
Using the concepts reviewed so far in this textbook, do the following:
1. Name a health problem (for example, new HIV infections in the U.S., Opioid Use, etc.
2. Describe interventions for the health problem that you have identified:
The Health System in the United States
As mentioned at the beginning of this chapter, in the year 2022, the health system in the U.S. is a $4.3 trillion business (I am using here the word, 'business' although some people don't like to use it when referring to a system that is created to serve people). [19]. This health system is expected to cover and respond to the needs of a nation that has a population of 333,287,557 million people, [20]in which a great number of them are over the age of 65. Add to this picture is the fact that the response of this system has to be designed in a way that respond to a growing number of ethnic and racial diverse group of people seeking health care services. These two mentioned elements are enough to overwhelmed a system that does not have all of the resources for preventive and curative health, or, the resources are insufficient. In this context and using the Health of the U.S. report from CDC,[21] a review of the information (mainly numerical data) will be presented with the purpose of giving the reader an overall picture of the current situation of the health care system in the U.S. and its people.
National Health expenditure
In the U.S., How much of the Gross Domestic Product (GDP) is spend in health?
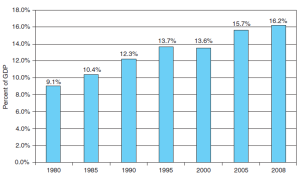 Percent of US National Gross Domestic Expenditures Spent for Health-Related Purposes, Selected Years, 1980-2008 Percent of US National Gross Domestic Expenditures Spent for Health-Related Purposes, Selected Years, 1980-2008 |
| Text Figure 3-6. Source: Data from Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group; U.S. Department of Commerce, Bureau of Economic Analysis.
Find new data - New data entered Dec-31-22 below
"Total National Health Expenditure", Health System Tracker, Public Domain. |
How much of the National health expenditure is for public health? Or, what is the budget's distribution?
 |
| update later
"Total National Health Expenditure", Health System Tracker, Public Domain.
"Personal Healthcare expenditures y source of funds", Centers for Medicare & Medicaid Services, National Health Expenditures Accounts, Public domain. Keep source below just for future needs See Sources and Definitions, National Health Expenditure Accounts (NHEA) and Health, United States, 2020–2021 Table HExpPers. |
 |
| Text Figure 3-7. Source: Data from Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group.
Find new data - |
National Health care utilization
A great number of the health care system's budget in the U.S. is utilized to serve an aging and diverse population, representing a
Knowing how much is assigned for public health service, it is important to review what are the services offered by the public health system in the U.S.
Essential Public Health Services (EPHS)
The following are the public health services that are considered essential, from these other subprograms derive.
In a graphic form, the EPHS are represented in a wheel of services:
 |
| Essential Public Health Services (EPHS) wheel |
These graphic representation also introduces the three major public health activities: Assurance, Assessment and Policy Development, which will be developed in content later [or, presented later also in another chapter, introduction to public health].
Public Health Activity and the Essential Public Health Services (EPHS)
From the assigned budgetary expenditure, how much of the public health activity and EPHS is assigned and spent by government level? See graph:
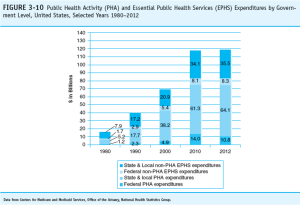 |
| Update this later |
Examine the web sites of these major health organizations: American Medical Association, American Hospital Association, American Nurses Association, and the American Association of Medical Colleges. Do your selections in the previous exercise differ from the priority issues of these organizations? How do you explain or account for any differences between the two lists?
“The nation’s population is growing and aging, and as we continue to address population health goals like reducing obesity and tobacco use, more Americans will live longer lives. These factors and others mean we will need more doctors,” the president of the AAMC and CEO (said. [24]
What is the importance of the above mentioned trends? It means that in terms of health care services, the demand will be focused more on those two major groups, the very young population and the group of older adults who will be highly diverse putting more demand on services that should be more culturally appropriate in terms of language and culture, just two mention two major need among diverse populations in the United States. Also, if the U.S. population is aging is because people in the U.S. are living longer (greater life expectancy as reviewed before in this chapter) and also more chronic diseases associated with obesity and tobacco use will be on demand for treatment and control at the level of the healthcare system and services, which also mean that more physicians and nurses will be needed in the near future to respond to these needs
The next section is health care resources -
The role of the health care providers especially, physicians and nurses
Also, the role of insurance companies and its healthcare plans offered to the population.
Models (examples of delivery of services) as part of the resources.
Resources in Healthcare: health care providers
Another important area of the public health care system is the supply of health care resources, how much is available for the consumer, and how much is affordable for the population? One important element related to the resources in healthcare is the number of health care providers such as physicians and nurses available for the care of the population. The current numbers and projections of the number of physicians and nurses in the U.S. healthcare system show a shortage. See some of the numbers presented in the images below - first, for physicians and second image is for nurses.
 |
| "National Physician Shortage," Image from pbs media, no license stated. |
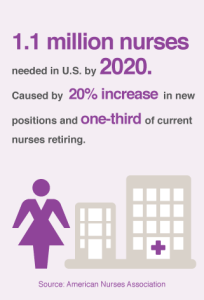 |
| "1.1 million nurses needed in U.S. by 2020," Image from healthline.com, no license stated. |
Physicians: Contradictory numbers
Physicians in the U.S. had increased in number from two sources: 1) the number of medical graduates from U.S. medical schools had increased in recent years [but not enough to cover the needs of the population] and, 2) the constant flow of foreign graduates physicians that have immigrated to the U.S., and obtained a license to practice in the U.S. That said, this information is contradictory, because as the graphs have show above, the number of physicians in the U.S. show a shortage, and the explanation is that there will not be enough physicians for the projected grow of the population in the next decades. And, additional reason for the decline of the number of physicians in the U.S. in the near future is due to the fact that a great number of current practitioners will be retiring soon, with no immediate replacement from the graduate medical schools or, international flow of foreign graduated that obtained their license to practice medicine in the U.S.[25]
Nurses: more are needed
The shortage of nurses is very similar to the one discussed above about the number of physicians in the U.S., but there is one great difference, no matter how many nurses could come from abroad and get licensed in the U.S., augmented with the number of nurses graduated from U.S. nurses' schools, the shortage of nurses, faculty to train nurses and resource still be great. There is need for more nurses in the country.[26]
Other health care professionals
Laboratory and imaging technicians, Anesthesiologists, Pharmacists, Physical therapy, etc. these will be discussed in the next chapter about the US public health work force.
Trends in terms of disease
“The nation’s population is growing and aging, and as we continue to address population health goals like reducing obesity and tobacco use, more Americans will live longer lives. These factors and others mean we will need more doctors,” Kirch said. https://www.fiercehealthcare.com/practices/physician-shortage-numbers-keep-climbing-now-estimated-at-122k-by-2032
In the past decades, the number of physicians in the country had increased in recent years, this is not the same for the number of registered nurses that is experiencing a shortage, not only in terms of diversity but also in terms of numbers in general.
Physicians in the U.S. had increased in number (how many per inhabitant?) as part of the increased number of medical graduates from U.S. medical schools, but also for the greater numbers of foreign graduates that have immigrated to the U.S. and that are now practitioners in the U.S., without the intention to create confusion, the projected
it is important to note also that the majority of physicians prefer to work on specialties making the generalist and the family care professional less in terms of numbers, primary care physicians had not have increased in recent decades, creating a gap between specialist services and family practice, although the country needs more primary care providers. -- revise the terms, make sure is uniform, and find the data to support the statements.
health care practices – this happens a lot among many diabetic patients who don’t receive the right evidence-based care for such chronic conditions such as high blood pressure, diabetes and heart disease. Third, another terms that is not commonly heard of is the term, misuse? Misuse which is another way of describing medical errors frequently occurs for example, when a patient doesn’t fully benefit from a
treatment because of a preventable problem – or when a patient is harmed by a treatment. [27] The literature reports that between 44,000 and 98,000 people die annually from preventable errors.[28] Especially for those people who are afraid about overuse of the system as it was mentioned at the beginning of this section, contrary to what most people think, underused of care is actually a greater problem than overuse. [29]
After reading about use of health services and the terms, overuse, underused and misuse, what do you think are the main reasons for each one of the these categories, make a list of these reasons and discuss/share your answers in a small group with your classmates.
This chapter is more about how the public health system is organized in the U.S. mostly chapter 3 in Turnock's book
Learning Objectives
By the end of this chapter, the learner will be able to
-
Learn about the programs and services that constitute what is known as the 'public health system' in the United States
- Learn about importance of public health programs and services in the U.S.
- Learn about the structure/components of the public health programs and services in the U.S.
- List the major assessment tools used to evaluate the proper functioning, and efficiency of most common public health program and services
- Link the public health program and services with the Healthy People 2030 Objectives and identify its commonalities
- Provide examples of successful public health program and services in the U.S. by identifying those elements that make these programs successful
Chapters' overview -
The United States Health System
One of the major objectives of this chapters is to Learn about the programs and services that constitute what is known as the 'public health system' in the United States. In general, it is accepted that the health system includes public health because of the importance of prevention, but in reality, the Health System in the United States is highly focused on health care services that are mostly curative) and that require about $4.3 trillion or $12,914 per person in 2022 (In the context of the nation's Gross Domestic Product (GDP), health spending accounted for 18.3%).[30]. As said before, one of the difficulties in the health care system in the U.S. is that prevention is not always part of the "health services" provided to people but since there is an important distinction between curative and preventive health care, the following terms need to be reviewed for a better understanding of the content of this chapter, and related overall content of the book.
Understanding Prevention and Health Services in the U.S.
 |
| Make my own or, find the source - which I could not find it yet as Dec. 27, 2022 |
In general, the term refers to activities that attempt to modify human behaviors to reduce those known to affect adversely the ability to resist disease, or, injury-inducing factors, thereby eliminating exposures to harmful factors. Or, as the World Health Organization (WHO) defines the term, Health promotion is "[T]he process of empowering people to increase control over their health and its determinants through health literacy efforts and multisectoral action to increase healthy behaviors."[32]
 |
| Health Promotion (Word Cloud). Find source later. To see details of the image including content, right click and choose, open image in new tab. |
Examples of health promotion include: activities for the community-at-large or for populations at increased risk of negative health outcomes. Health promotion usually addresses behavioral risk factors such as tobacco use, obesity, diet and physical inactivity, as well as the areas of mental health, injury prevention, drug abuse control, alcohol control, health behavior related to HIV, and sexual health.
In general, it can be considered as part of health promotion. Health protection refers to specific protection activities that provide individuals with resistance to factors (such as bacteria and viruses), or, modify environments to decrease potentially harmful interactions of health influencing factors (such as toxic exposures in the workplace).
 |
| Health Protection. Find source info later. |
Examples of health protection include the use of seat belts while driving, using helmets at work to protect for some environmental exposures, or, injuries. The use of vaccines is another common example of health protection, and preventive treatment with antibiotics for example in the case of family members exposed to tuberculosis but who had not present symptoms of the disease, or, who don't have active tuberculosis.
Early Case Finding and Prompt Treatment, Disability Limitation, and Rehabilitation
Early Detection and Case Finding
How are the cases found? Assuming that the definition of what constitute a 'case' for a specific problem or, health issue is defined (an information usually provided by medical textbooks or, directly from the Centers for Disease and Controls in the U.S.). The 'case finding' will be conducted by finding those individual who meet the disease/condition criteria (detected frequently from the screening); once this is done, these became the ‘cases.
Prompt Treatment, Disability Limitation, and Rehabilitation
From its beginning to end, each disease has a natural course (or, 'natural history'). This can be observed if no medical intervention is taken and the disease is allowed to run its full course. Although this concept is commonly found in an epidemiology textbook (see chapter 1 in my epidemiology textbook for an extended version of this concept), it is presented here in order to provide a context to the information that can be useful for all kinds of public health professionals. The following image summarizes (and, outlines) the main components of the natural history of disease.
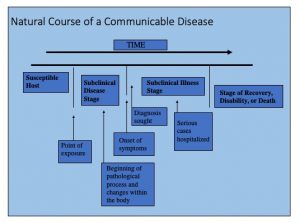 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
This model (of natural history of disease) has been used to develop the concepts of primary, secondary and tertiary prevention that is commonly used in medicine, public health and especially in public health education. Please note that the model applies mainly to the study of infectious, or, communicable diseases, it does not help much in the study of non-communicable (or, non-infectious) diseases.
Examples of Primary Prevention include, the use of pap smear to prevent and detect early stages of cervical cancer, mammograms, digital rectal exams, colonoscopies, and other common screening tests. The idea is to identify the risk, or, the disease in an early stage mostly before symptoms develop.
Secondary Prevention is the most expensive stage because the cases that are serious or, need intense treatment are hospitalized to receive a more intensive intervention, those cases that are not hospitalized are usually given treatment under supervision especially for middle cases of a disease. In the secondary prevention step, the person recovers or die. If the person survives and became disabled, then, the individual enters the tertiary level of prevention, which is next.
This phase is commonly misunderstood because many people see rehabilitation as part of the secondary prevention in which only medical care professionals provide services to rehabilitate the affected individual, but in general, going beyond the medical model, rehabilitation is more than just medical care, many times it means, helping the affected individual to improve the quality of life and to come back to society in a productive manner.
In addition, the following table provides additional details including examples that should help to understand the above mentioned concepts:
 |
| Image prepared by Giovanni Antunez, Licensed CC BY 4.0 |
The levels of prevention can be linked to the clinical model, and this helps to put into context the common medical and public health interventions that most people are used to be seen as part of the work of the medical and public health work. See a summary of this comparison in the following table:
| In the clinical model, there are three levels of health care services | In the public health model, there are three level of prevention |
| Primary care | Primary prevention |
| Secondary care | Secondary prevention |
| Tertiary care | Tertiary prevention |
Important comments about the information above
The above distinctions should help public health professionals in training, especially health educators to better understand the differences between the levels of care and the level of prevention, especially for students who are not familiar with the United States healthcare system. This system works differently in other parts of the world, especially in developing countries. So, the comparison should also help to conciliate the differences.
Applying the content...
Using the concepts reviewed so far in this textbook, do the following:
1. Name a health problem (for example, new HIV infections in the U.S., Opioid Use, etc.
2. Describe interventions for the health problem that you have identified:
The Health System in the United States
As mentioned at the beginning of this chapter, in the year 2022, the health system in the U.S. is a $4.3 trillion business (I am using here the word, 'business' although some people don't like to use it when referring to a system that is created to serve people). [34]. This health system is expected to cover and respond to the needs of a nation that has a population of 333,287,557 million people, [35]in which a great number of them are over the age of 65. Add to this picture is the fact that the response of this system has to be designed in a way that respond to a growing number of ethnic and racial diverse group of people seeking health care services. These two mentioned elements are enough to overwhelmed a system that does not have all of the resources for preventive and curative health, or, the resources are insufficient. In this context and using the Health of the U.S. report from CDC,[36] a review of the information (mainly numerical data) will be presented with the purpose of giving the reader an overall picture of the current situation of the health care system in the U.S. and its people.
National Health expenditure
In the U.S., How much of the Gross Domestic Product (GDP) is spend in health?
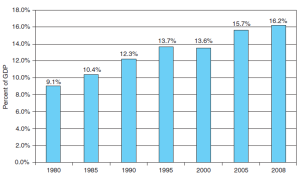 Percent of US National Gross Domestic Expenditures Spent for Health-Related Purposes, Selected Years, 1980-2008 Percent of US National Gross Domestic Expenditures Spent for Health-Related Purposes, Selected Years, 1980-2008 |
| Text Figure 3-6. Source: Data from Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group; U.S. Department of Commerce, Bureau of Economic Analysis.
Find new data - New data entered Dec-31-22 below
"Total National Health Expenditure", Health System Tracker, Public Domain. |
How much of the National health expenditure is for public health? Or, what is the budget's distribution?
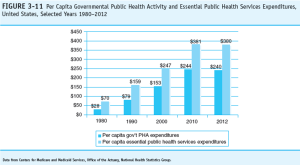 |
| update later
"Total National Health Expenditure", Health System Tracker, Public Domain.
"Personal Healthcare expenditures y source of funds", Centers for Medicare & Medicaid Services, National Health Expenditures Accounts, Public domain. Keep source below just for future needs See Sources and Definitions, National Health Expenditure Accounts (NHEA) and Health, United States, 2020–2021 Table HExpPers. |
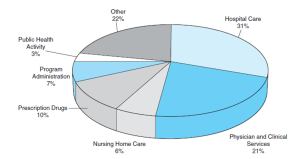 |
| Text Figure 3-7. Source: Data from Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group.
Find new data - |
National Health care utilization
A great number of the health care system's budget in the U.S. is utilized to serve an aging and diverse population, representing a
Knowing how much is assigned for public health service, it is important to review what are the services offered by the public health system in the U.S.
Essential Public Health Services (EPHS)
The following are the public health services that are considered essential, from these other subprograms derive.
In a graphic form, the EPHS are represented in a wheel of services:
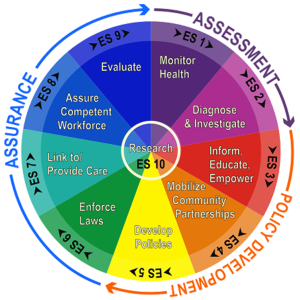 |
| Essential Public Health Services (EPHS) wheel |
These graphic representation also introduces the three major public health activities: Assurance, Assessment and Policy Development, which will be developed in content later [or, presented later also in another chapter, introduction to public health].
Public Health Activity and the Essential Public Health Services (EPHS)
From the assigned budgetary expenditure, how much of the public health activity and EPHS is assigned and spent by government level? See graph:
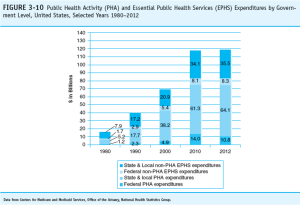 |
| Update this later |
Examine the web sites of these major health organizations: American Medical Association, American Hospital Association, American Nurses Association, and the American Association of Medical Colleges. Do your selections in the previous exercise differ from the priority issues of these organizations? How do you explain or account for any differences between the two lists?
What is the importance of the above mentioned trends? It means that in terms of health care services, the demand will be focused more on those two major groups, the very young population and the group of older adults who will be highly diverse putting more demand on services that should be more culturally appropriate in terms of language and culture, just two mention two major need among diverse populations in the United States. Also, if the U.S. population is aging is because people in the U.S. are living longer (greater life expectancy as reviewed before in this chapter) and also more chronic diseases associated with obesity and tobacco use will be on demand for treatment and control at the level of the healthcare system and services, which also mean that more physicians and nurses will be needed in the near future to respond to these needs
The next section is health care resources -
The role of the health care providers especially, physicians and nurses
Also, the role of insurance companies and its healthcare plans offered to the population.
Models (examples of delivery of services) as part of the resources.
Resources in Healthcare: health care providers
Another important area of the public health care system is the supply of health care resources, how much is available for the consumer, and how much is affordable for the population? One important element related to the resources in healthcare is the number of health care providers such as physicians and nurses available for the care of the population. The current numbers and projections of the number of physicians and nurses in the U.S. healthcare system show a shortage. See some of the numbers presented in the images below - first, for physicians and second image is for nurses.
 |
| "National Physician Shortage," Image from pbs media, no license stated. |
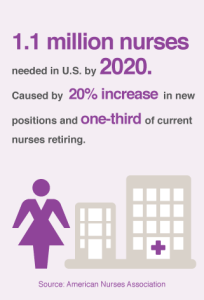 |
| "1.1 million nurses needed in U.S. by 2020," Image from healthline.com, no license stated. |
Physicians: Contradictory numbers
Physicians in the U.S. had increased in number from two sources: 1) the number of medical graduates from U.S. medical schools had increased in recent years [but not enough to cover the needs of the population] and, 2) the constant flow of foreign graduates physicians that have immigrated to the U.S., and obtained a license to practice in the U.S. That said, this information is contradictory, because as the graphs have show above, the number of physicians in the U.S. show a shortage, and the explanation is that there will not be enough physicians for the projected grow of the population in the next decades. And, additional reason for the decline of the number of physicians in the U.S. in the near future is due to the fact that a great number of current practitioners will be retiring soon, with no immediate replacement from the graduate medical schools or, international flow of foreign graduated that obtained their license to practice medicine in the U.S.[40]
Nurses: more are needed
The shortage of nurses is very similar to the one discussed above about the number of physicians in the U.S., but there is one great difference, no matter how many nurses could come from abroad and get licensed in the U.S., augmented with the number of nurses graduated from U.S. nurses' schools, the shortage of nurses, faculty to train nurses and resource still be great. There is need for more nurses in the country.[41]
Other health care professionals
Laboratory and imaging technicians, Anesthesiologists, Pharmacists, Physical therapy, etc. these will be discussed in the next chapter about the US public health work force.
Trends in terms of disease
If people are living longer, then, chronic diseases became the norm for the elder population, and these diseases are related to two main factors among others, obesity and tobaccon use (in the present, but mostly in the past during young age). As the
“The nation’s population is growing and aging, and as we continue to address population health goals like reducing obesity and tobacco use, more Americans will live longer lives. These factors and others mean we will need more doctors,” Kirch said. https://www.fiercehealthcare.com/practices/physician-shortage-numbers-keep-climbing-now-estimated-at-122k-by-2032
In the past decades, the number of physicians in the country had increased in recent years, this is not the same for the number of registered nurses that is experiencing a shortage, not only in terms of diversity but also in terms of numbers in general.
Physicians in the U.S. had increased in number (how many per inhabitant?) as part of the increased number of medical graduates from U.S. medical schools, but also for the greater numbers of foreign graduates that have immigrated to the U.S. and that are now practitioners in the U.S., without the intention to create confusion, the projected
it is important to note also that the majority of physicians prefer to work on specialties making the generalist and the family care professional less in terms of numbers, primary care physicians had not have increased in recent decades, creating a gap between specialist services and family practice, although the country needs more primary care providers. -- revise the terms, make sure is uniform, and find the data to support the statements.
health care practices – this happens a lot among many diabetic patients who don’t receive the right evidence-based care for such chronic conditions such as high blood pressure, diabetes and heart disease. Third, another terms that is not commonly heard of is the term, misuse? Misuse which is another way of describing medical errors frequently occurs for example, when a patient doesn’t fully benefit from a
treatment because of a preventable problem – or when a patient is harmed by a treatment. [42] The literature reports that between 44,000 and 98,000 people die annually from preventable errors.[43] Especially for those people who are afraid about overuse of the system as it was mentioned at the beginning of this section, contrary to what most people think, underused of care is actually a greater problem than overuse. [44]
After reading about use of health services and the terms, overuse, underused and misuse, what do you think are the main reasons for each one of the these categories, make a list of these reasons and discuss/share your answers in a small group with your classmates.
EPHS refers to those services considered essential (the basic and necessary).
In the United States, the term refers to changes in demographics trend especially age (a great number of older adults) compared to a small percent of the younger population.
The separation between older adults (65 and more) and young (under 18 years) individuals that is becoming more accentuated.
the term refers to something that is designed to be practical and useful, rather than attractive.